What’s the difference between gastric bypass and sleeve gastrectomy?
If you’re considering bariatric surgery, you’ve probably heard two names over and over: gastric bypass and sleeve gastrectomy. They’re the two most common weight loss surgeries in the U.S., and for good reason. Both help people lose significant weight when diet and exercise haven’t worked. But they work in very different ways-and the choice isn’t just about which one loses more weight. It’s about your body, your health, your lifestyle, and what you’re willing to live with long-term.
How each procedure actually works
Gastric bypass, or Roux-en-Y gastric bypass, is like rerouting your digestive system. Surgeons create a small stomach pouch-about the size of a golf ball-and connect it directly to the middle part of your small intestine. That means food skips most of your stomach and the first section of your intestine. This does two things: it limits how much you can eat, and it reduces how many calories your body absorbs. The typical Roux limb is around 119 cm long, and the biliary limb is about 58 cm. This rerouting changes how your body handles food, which is why it often leads to faster and greater weight loss.
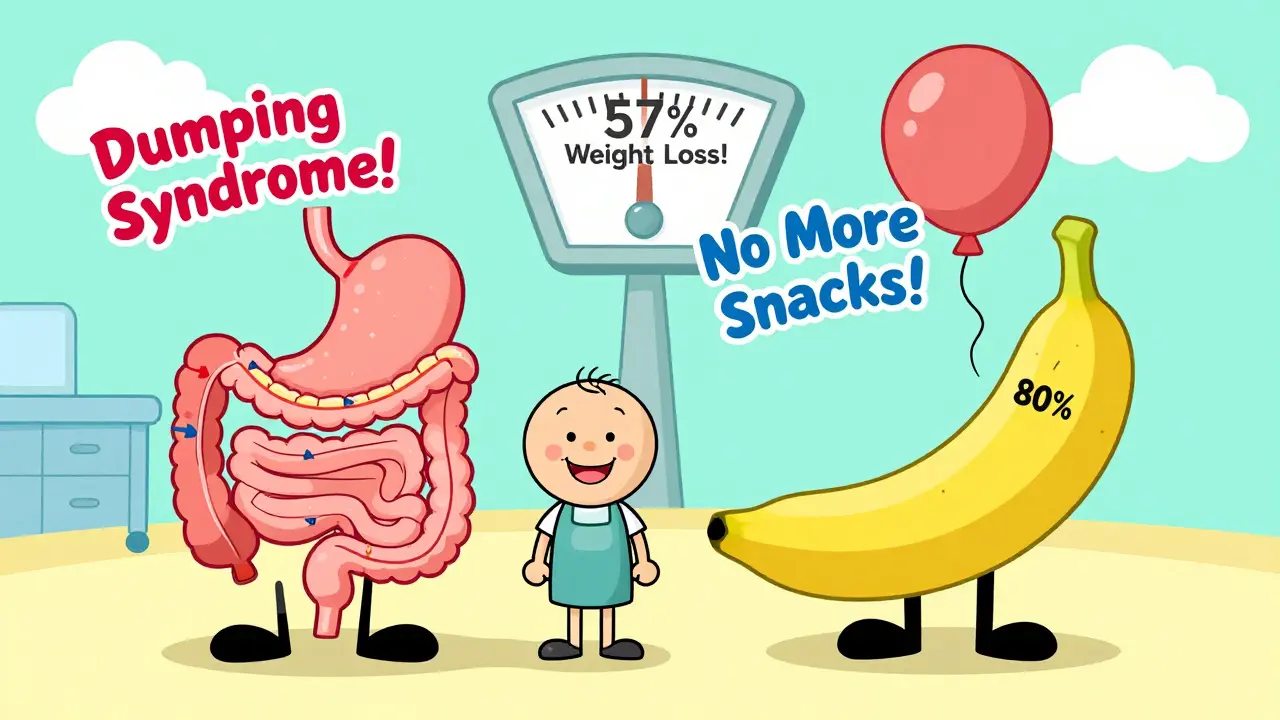
Sleeve gastrectomy is simpler. About 80% of your stomach is removed, leaving a thin, banana-shaped tube-hence the name “sleeve.” This new stomach holds only 2 to 5 ounces of food. It doesn’t reroute anything. It just makes you feel full faster. The procedure takes about 47 minutes on average, compared to 68 minutes for gastric bypass. That’s not just a time difference-it means fewer chances for complications during surgery.
Weight loss: Which one works better?
If your main goal is to lose the most weight possible, gastric bypass usually wins-at least in the first few years. Studies show that after five years, gastric bypass patients lose about 57% of their excess weight, while sleeve gastrectomy patients lose around 49%. Some data from UPMC shows gastric bypass patients losing 60-80% of excess weight within 18 months, while sleeve patients lose 60-70% over the same period, but more slowly.
But here’s the catch: weight loss isn’t just about the number on the scale. Gastric bypass also changes your hunger hormones more dramatically. That means less cravings, more fullness, and better control over eating. Sleeve gastrectomy helps too, but many patients report feeling hungrier long-term, even after losing weight.
What about health improvements?
Both surgeries dramatically improve or even reverse obesity-related conditions like type 2 diabetes, high blood pressure, sleep apnea, and fatty liver disease. But gastric bypass tends to be more effective for diabetes. That’s because the rerouting of the intestine triggers changes in gut hormones that help your body regulate blood sugar better. Studies show diabetes resolution rates are higher with bypass-sometimes over 80% within a year.
For high blood pressure and cholesterol, gastric bypass also shows stronger results. One 2024 JAMA study found that hypertension improved more often in bypass patients than in sleeve patients. That doesn’t mean sleeve doesn’t help-it does. But if you’re struggling with diabetes or metabolic syndrome, bypass might give you a stronger edge.
Risks and complications: What you’re signing up for
No surgery is risk-free. But the risks are different for each procedure.
Gastric bypass has a higher risk of serious complications. It’s more complex, so there’s more room for things to go wrong during or after surgery. Long-term, it can cause vitamin and mineral deficiencies-especially in B12, iron, calcium, and folate. That’s because your body can’t absorb them as well without the bypassed sections of your stomach and intestine. You’ll need lifelong supplements and regular blood tests-at least twice a year.
Sleeve gastrectomy is safer in the short term. Studies show a 32.8% lower risk of death within five years compared to bypass. Hospital stays are similar-about one day for both-but recovery is often easier. There’s no rerouting, so nutrient absorption stays mostly normal. You’ll still need supplements, but usually just once a year for monitoring.
But sleeve has its own problems. One big one is reflux. About 20-30% of sleeve patients develop or worsen GERD after surgery. Gastric bypass, on the other hand, often improves reflux. Another issue: revision rates. More sleeve patients end up needing another surgery later. A 2022 study of over 95,000 people found that 5-year revision rates were 3.2 percentage points higher for sleeve than bypass. Why? Weight regain, stomach stretching, or unresolved reflux can push people back to the operating room.
Life after surgery: What daily life looks like
After either surgery, you’ll need to change how you eat. You’ll eat smaller meals, chew slowly, avoid sugary drinks, and never skip protein. But the restrictions are tighter with gastric bypass.
If you eat too much sugar or fat after bypass, you might get “dumping syndrome.” That’s when food rushes too fast into your intestine. Symptoms include nausea, sweating, dizziness, cramps, and diarrhea. It happens in 50-70% of bypass patients. It’s not dangerous, but it’s unpleasant-and it teaches you to avoid certain foods. Many people say it’s the best deterrent against unhealthy eating.
Sleeve patients don’t get dumping syndrome. But they might struggle with hunger. Without the hormonal changes of bypass, some people feel hungry more often, even if their stomach is small. That’s why long-term success with sleeve often depends on behavior change, not just surgery.
On Reddit’s r/bariatrics, people who had sleeve say things like, “I recovered faster, but I still crave snacks.” Those who had bypass say, “I couldn’t eat junk even if I wanted to.” Both are true.
Cost and insurance: What you’ll pay
Insurance usually covers both procedures if you meet the NIH criteria: BMI ≥40, or BMI ≥35 with at least one obesity-related condition like diabetes or high blood pressure. Some insurers, like UnitedHealthcare, now require BMI ≥45 as of 2024.
Out-of-pocket costs vary, but as of late 2024, sleeve gastrectomy averages $14,500 after insurance pays its 80%, while gastric bypass averages $19,300. That’s about a 25% difference. The higher cost of bypass comes from longer surgery time, more complex aftercare, and higher risk of complications requiring follow-up care.
Both require the same pre-op steps: six months of documented weight loss attempts, a psychological evaluation, and medical clearance. You won’t be approved unless you’ve tried other methods first.
Why sleeve gastrectomy is now the most popular
In 2010, sleeve gastrectomy made up less than 10% of bariatric surgeries. By 2023, it was over 63%. Gastric bypass dropped from 31% to 27% in the same period.
Why? Simplicity. Safety. Faster recovery. Fewer supplements. Lower upfront risk. Patients and surgeons both prefer it-especially when they’re unsure about lifelong nutrient monitoring. It’s also easier to perform, so more surgeons are trained in it.
But popularity doesn’t always mean best. The rise of sleeve is partly because it’s easier to sell. It sounds less invasive. But for people with severe diabetes or those who need maximum weight loss, bypass is still the gold standard.
What’s next? Hybrid procedures and future options
Surgeons are now testing hybrid procedures that combine elements of both. Think of it as a “mini-bypass” or a “sleeve with bypass.” Early results from Mayo Clinic and Massachusetts General show promise: better weight loss than sleeve alone, fewer nutrient issues than full bypass.
For people who’ve had sleeve and regained weight, new endoscopic options are emerging-like placing a sleeve-reducing device through the mouth, without open surgery. About 15% of sleeve patients may need some kind of revision within five years.
The future isn’t just about picking one surgery. It’s about matching the right tool to the right person.
Which one is right for you?
There’s no universal answer. But here’s a simple guide:
- Choose gastric bypass if: You have type 2 diabetes, severe metabolic syndrome, or need the most weight loss possible. You’re willing to take lifelong supplements and avoid sugar/fat to prevent dumping syndrome. You’re okay with a slightly higher risk of complications.
- Choose sleeve gastrectomy if: You want a simpler, faster surgery with fewer long-term nutrient issues. You’re confident you can manage hunger with diet and behavior changes. You’re concerned about surgery risks or don’t want to deal with dumping syndrome.
Both work. Both change lives. But one might fit your body, your health, and your future better than the other.
Can you reverse gastric bypass or sleeve gastrectomy?
Gastric bypass is technically reversible, but it’s rarely done. Reversing it means reattaching the stomach and intestine, which is complex and risky. Sleeve gastrectomy, on the other hand, is permanent-you’ve removed 80% of your stomach. You can’t put it back.
Which surgery has fewer side effects?
Sleeve gastrectomy generally has fewer long-term side effects. It doesn’t cause malabsorption, so vitamin deficiencies are less common. It also doesn’t cause dumping syndrome. But it has a higher chance of worsening reflux and needing revision surgery later. Gastric bypass causes more immediate side effects like dumping and nutrient issues, but fewer revisions over time.
Do you need to take supplements forever?
Yes-for both surgeries, but more so for gastric bypass. Sleeve patients usually need a daily multivitamin, calcium, and vitamin D once a year. Bypass patients need daily B12, iron, calcium, vitamin D, and often folate and zinc. Blood tests every six months are required for bypass patients to catch deficiencies before they cause anemia or nerve damage.
Can you gain weight back after either surgery?
Yes, and it’s more common with sleeve gastrectomy. About 15-20% of sleeve patients regain significant weight within five years, often due to stomach stretching or returning to old eating habits. Gastric bypass patients are less likely to regain weight because of the hormonal changes and dumping syndrome acting as natural deterrents. But weight regain can still happen if you ignore dietary rules.
Is one surgery better for older adults?
For patients over 60, sleeve gastrectomy is often preferred because it’s less invasive and carries a lower risk of complications and death. Gastric bypass’s higher risk profile makes it less ideal for older patients unless they have severe diabetes or need maximum weight loss. Age alone doesn’t disqualify anyone, but safety becomes a bigger factor.

Comments (14)
Sawyer Vitela
25 Jan, 2026Sleeve is just a lazy man's bypass. You think you're avoiding complications? Nah. You're just setting yourself up for a 3am snack run and a revision surgery in 5 years. The data doesn't lie.
Dolores Rider
25 Jan, 2026They're hiding something. Why do you think the FDA pushed sleeve so hard after 2015? Big Pharma wants you on lifelong supplements so they can sell you B12 vials for $200 a bottle. It's a money scheme. I saw a whistleblower video on 4chan.
Alexandra Enns
26 Jan, 2026I'm Canadian and I'm telling you, the US medical system is a circus. Sleeve is cheaper because they don't want to pay for the follow-ups. They're outsourcing your nutrient deficiencies to Walmart vitamins. We don't do this nonsense up here. We have real healthcare.
Amelia Williams
27 Jan, 2026I had sleeve in 2021 and honestly? I thought I'd be starving forever. But the hunger faded. It's not magic, but it's real. I lost 110 lbs and I'm not on 12 supplements. You don't need to suffer to heal. 🙏
Himanshu Singh
29 Jan, 2026The body is not a machine to be rewired. Both surgeries are tools, but the real surgery happens in the mind. Who are you when you can't eat like before? That's the question no one asks. 🌱
Jenna Allison
29 Jan, 2026Dumping syndrome isn't just 'unpleasant' - it's a physiological feedback loop that rewires reward pathways. Bypass isn't just restrictive, it's neurochemical. That's why relapse rates are lower. It's not willpower. It's biology.
Viola Li
31 Jan, 2026I'm sorry, but if you're choosing surgery because you 'couldn't lose weight with diet' - you're just giving up. I lost 80 lbs with intermittent fasting and walking. No scalpel needed. You're enabling a culture of quick fixes.
Darren Links
1 Feb, 2026I had bypass in 2020. The first 6 months were brutal. No sugar. No caffeine. No pizza. But now? I eat a salad and feel full. My diabetes is gone. I don't miss the junk. It's not about restriction - it's about clarity.
Marie-Pier D.
2 Feb, 2026To anyone scared of the long-term stuff - you're not alone. I cried the first time I had to swallow a B12 shot. But my sister had sleeve and now she's back on metformin. We both needed help. Neither of us are weak. 💕
Shanta Blank
4 Feb, 2026Sleeve patients are just walking time bombs with a banana stomach. They think they're safe? HA. Five years later, they're back in the ER with a ruptured staple line and a $120k bill. Bypass is the only honest choice. The rest is denial.
venkatesh karumanchi
5 Feb, 2026I'm from India. We don't have access to this stuff. But I read everything. I think the real issue is not which surgery - it's that we treat obesity like a personal failure. It's a disease. We need better access. Not more judgment.
Kat Peterson
6 Feb, 2026I had the sleeve. I looked in the mirror and thought, 'I'm not a monster anymore.' Then I got a tattoo of a banana on my ribcage. I'm not sorry. This journey is art. And I'm the masterpiece. 🍌✨
Tiffany Wagner
6 Feb, 2026i had bypass 3 years ago and honestly i dont even think about food the way i used to its just different now and the dumping thing is wild like one time i ate a cookie and i felt like i was gonna die but then i was fine just so weird
Darren Links
8 Feb, 2026I saw someone say they lost weight with fasting. That’s great for some. But if you have BMI 50 and diabetes? Fasting won’t save you. Surgery isn’t giving up - it’s choosing to live.