If you’ve been lying awake for hours, night after night, for months or even years, you’re not just tired-you’re trapped. Chronic insomnia isn’t just trouble falling asleep. It’s waking up too early, not feeling rested, dreading bedtime, and carrying that exhaustion into every part of your day. And if you’ve tried drinking chamomile tea, turning off your phone, or wearing sleep masks, only to find yourself still wide awake at 2 a.m., you’re not failing. You’re just using the wrong tools.
What Chronic Insomnia Really Means
Chronic insomnia isn’t a bad night or two. The American Academy of Sleep Medicine defines it clearly: trouble falling asleep, staying asleep, or waking up too early-happening at least three nights a week for three months or longer. It’s not about being stressed or having a busy mind. It’s a biological loop that keeps your brain stuck in alert mode, even when your body is exhausted.
This isn’t normal aging. It’s not just "being a light sleeper." It’s a condition that rewires how your brain responds to bedtime. And the worst part? Most people are told to "just relax" or "try better sleep hygiene," which doesn’t fix the root problem.
Why Sleep Hygiene Isn’t Enough
Sleep hygiene sounds simple: no caffeine after noon, keep your room cool, avoid screens before bed. These tips sound helpful-and they are, for people who have occasional trouble sleeping. But for chronic insomnia, they’re like putting a bandage on a broken bone.
Research from the American Academy of Sleep Medicine shows sleep hygiene alone has only moderate evidence of effectiveness. That means it might help a little, but it won’t fix the deep, ingrained patterns keeping you awake. Dr. Jack D. Edinger, one of the leading researchers in this field, puts it bluntly: "Sleep hygiene education alone is minimally effective for chronic insomnia and should not be offered as standalone treatment."
Why? Because chronic insomnia isn’t caused by a messy bedroom or too much coffee. It’s caused by learned behaviors and anxious thoughts that turn your bed into a place of frustration. You start associating your bed with lying awake, worrying, and feeling defeated. Your brain learns: "Bed = stress." And no amount of blackout curtains changes that.
The Only Treatment That Actually Works Long-Term
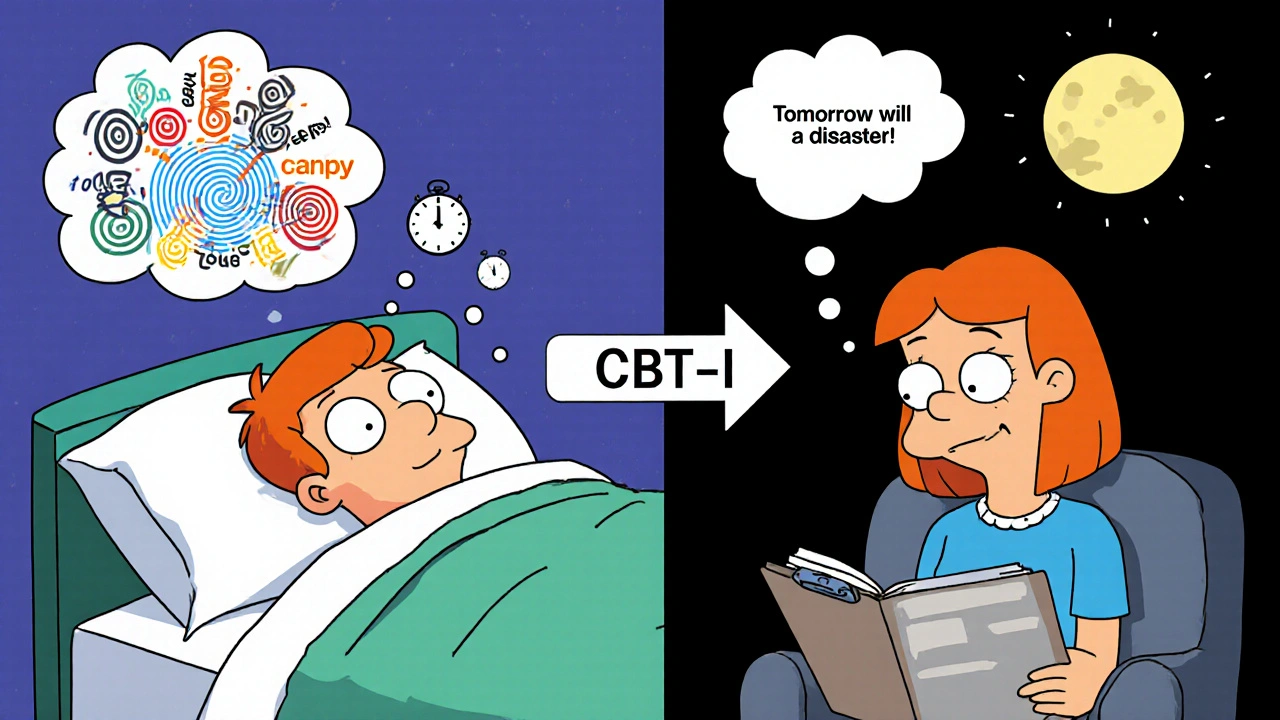
There’s one treatment that’s been proven again and again to work better than pills-for the long haul. It’s called Cognitive Behavioral Therapy for Insomnia, or CBT-I. It’s not a magic cure. It’s not quick. But it’s the only one that changes your brain’s relationship with sleep.
The American College of Physicians, the American Academy of Sleep Medicine, and the National Institutes of Health all recommend CBT-I as the first-line treatment for chronic insomnia. Not pills. Not supplements. Not melatonin. CBT-I.
Here’s what it does: it breaks the cycle. It doesn’t just help you sleep better-it helps you stop fearing sleep. And the results? Studies show 70-80% of people who complete CBT-I see clinically meaningful improvement. That’s not "a little better." That’s going from 4 hours of sleep to 7, from waking up 5 times a night to once, from dreading bedtime to actually feeling tired when it arrives.
What’s Inside CBT-I? (It’s Not What You Think)
CBT-I isn’t therapy where you talk about your childhood. It’s a structured, action-based program-usually 6 to 8 weekly sessions-with clear, specific steps. Here’s what it actually includes:
- Stimulus Control Therapy - Your bed is only for sleep and sex. If you’re not asleep in 15-20 minutes, you get up. Go to another room. Read under dim light. Don’t check your phone. Come back only when you’re sleepy. This retrains your brain: bed = sleep, not stress.
- Sleep Restriction - This sounds counterintuitive, but it works. If you’re only sleeping 5 hours a night, you’re allowed to be in bed only 5 hours. You set a fixed bedtime and wake time-even on weekends. You’re tired? Yes. For the first week or two, you’ll feel awful. But your sleep drive builds up. Your body starts to consolidate sleep. Within weeks, you’re sleeping more efficiently. Studies show this is one of the most powerful parts of CBT-I.
- Cognitive Restructuring - You start noticing the thoughts that keep you up: "I need 8 hours or I’ll fail at work," or "If I don’t sleep tonight, tomorrow will be a disaster." CBT-I helps you challenge those thoughts. You learn that your body can function on less sleep than you think. That anxiety about sleep is what’s keeping you awake-not the lack of sleep itself.
- Relaxation Training - Not just deep breathing. It’s progressive muscle relaxation, diaphragmatic breathing, and mindfulness techniques that lower your nervous system’s baseline arousal. You’re not trying to force sleep. You’re letting your body shift into rest mode.
- Sleep Hygiene (as a support, not the solution) - Yes, you still avoid caffeine after 2 p.m., keep your room around 65°F (18.3°C), and use blackout curtains. But now, these are just the small, supportive habits-not the main treatment.
CBT-I vs. Sleeping Pills: The Real Difference
You’ve probably tried sleeping pills. Zolpidem. Eszopiclone. Maybe even melatonin. They help-at first. But after 4 to 6 weeks, they stop working. And then you’re stuck: either take more, risk dependence, or go back to sleepless nights.
A 2020 meta-analysis in Sleep Medicine Reviews compared CBT-I to medication. Here’s what they found:
| Outcome | CBT-I Reduction | Medication Reduction |
|---|---|---|
| Sleep onset latency (time to fall asleep) | 18.2 minutes | 12.1 minutes |
| Wake after sleep onset (time awake during night) | 27.4 minutes | 15.8 minutes |
| Effect lasts 12 months after stopping | Yes | No |
CBT-I doesn’t just help you sleep better-it helps you stay better. The changes stick. Pills? They vanish the moment you stop taking them.
Digital CBT-I: Can an App Really Help?
What if you can’t find a therapist? There aren’t enough of them. In the U.S., there’s only about 0.5 certified CBT-I therapists per 100,000 people. Rural areas? Often zero.
But digital programs like Sleepio and SHUTi have changed the game. A 2021 JAMA Internal Medicine trial found these apps helped 50-60% of users reach remission-compared to just 15-20% in control groups. One FDA-cleared app, Somryst, showed 55.4% remission rates in clinical trials.
These aren’t meditation apps with sleep sounds. They’re structured CBT-I programs with daily exercises, sleep diaries, cognitive exercises, and personalized feedback. Some even sync with Fitbit or Apple Watch to adjust sleep windows based on your actual sleep data.
And yes-they work. One Reddit user wrote: "After 8 weeks of Sleepio, my sleep efficiency went from 68% to 89%. I fall asleep in 15 minutes now, not 2 hours."
The Hard Part: The First Few Weeks
Let’s be honest: CBT-I is hard. Especially sleep restriction. You’re told to limit your time in bed to 5 hours when you’re already exhausted. You’ll feel like a zombie for a week or two. That’s normal. That’s the point.
62% of people on Patient.info’s insomnia forum say the first two weeks were the worst. But those who stuck with it? 78% reported less daytime fatigue. One user said: "I cried the first week. But by week 5, I was sleeping through the night. I didn’t realize how much energy I’d lost until it came back."
Stimulus control is hard too. Getting out of bed when you’re tired feels unnatural. You worry you’ll never fall asleep. But every time you get up and come back only when sleepy, you’re rebuilding trust between your brain and your bed.

Who Benefits the Most?
CBT-I works for everyone with chronic insomnia-no matter your age, gender, or health status. Dr. Daniel Buysse at the University of Pittsburgh found it works just as well for older adults as it does for younger people. Effect sizes of 1.0-1.3 on the Insomnia Severity Index mean large, life-changing improvements.
It’s especially effective for perimenopausal women, where hormonal changes can trigger insomnia. The American Academy of Sleep Medicine now recommends CBT-I plus moderate exercise-not hormone therapy-as the first step.
Even people with depression, chronic pain, or PTSD respond well to CBT-I. It doesn’t cure those conditions, but it breaks the insomnia cycle that makes everything worse.
How to Get Started
You don’t need to wait for a miracle. Here’s how to begin:
- Track your sleep for 7-14 days. Write down when you get in bed, when you fall asleep, when you wake up, and how many times you woke up. Use a notebook or a simple app like Sleep Cycle or Sleep as Android.
- Calculate your average total sleep time. If you’re sleeping 5.5 hours a night, that’s your starting time in bed.
- Set a fixed wake-up time-no matter what. Even on weekends. This is the anchor.
- Only go to bed when sleepy. Don’t go to bed early to "try" to sleep.
- If you’re not asleep in 15-20 minutes, get up. Go to another room. Sit in a chair. Don’t turn on bright lights. Come back only when sleepy.
- Eliminate caffeine after 2 p.m. and alcohol after 7 p.m.
- Try a digital CBT-I program like Sleepio, SHUTi, or Somryst. Many are covered by insurance now.
What’s Next for Insomnia Treatment?
CBT-I is becoming the standard. Dr. Andrew Krystal predicts that within the next decade, 90% of chronic insomnia cases will be treated with CBT-I, and pills will be reserved for short-term use only.
AI is starting to personalize CBT-I even more. Apps are now adjusting sleep windows based on your wearable data. Insurance companies are slowly catching up-37% of Fortune 500 companies now offer CBT-I through employee wellness programs.
But the biggest change isn’t technological. It’s cultural. We’re finally moving away from the myth that sleep problems are just about willpower. They’re a medical condition. And there’s a proven, safe, lasting fix.
Can I just use melatonin or herbal sleep aids instead of CBT-I?
Melatonin and herbal supplements like valerian or chamomile might help with occasional sleep issues or jet lag, but they don’t address the learned behaviors and anxiety that drive chronic insomnia. Studies show they have minimal impact on long-term sleep maintenance. CBT-I is the only treatment proven to change the underlying patterns keeping you awake.
How long does it take to see results from CBT-I?
Most people start noticing small improvements in sleep efficiency within 2-4 weeks. But full benefits-like falling asleep faster, waking less often, and feeling rested-usually take 8-12 weeks of consistent practice. The first two weeks of sleep restriction are often the hardest, but they’re also the most critical.
Is CBT-I covered by insurance?
Coverage varies. In the U.S., some insurance plans cover CBT-I through licensed therapists or FDA-cleared digital apps like Somryst. However, only about 38% of recommended CBT-I sessions are currently covered, according to the National Sleep Foundation. Digital programs are often more affordable and increasingly included in employer wellness plans.
Can I do CBT-I on my own without a therapist?
Yes. Many people successfully complete CBT-I using structured digital programs like Sleepio or SHUTi, or workbooks from experts like Dr. Colleen Carney. The key is following the protocol exactly-especially sleep restriction and stimulus control. Self-guided CBT-I has been shown to be nearly as effective as in-person therapy in multiple studies.
What if I have a medical condition like sleep apnea?
CBT-I is not a substitute for treating underlying medical conditions. If you snore loudly, gasp for air at night, or feel excessively sleepy during the day, you should be screened for sleep apnea first. Once apnea is treated, CBT-I can still help with any remaining insomnia symptoms. Many people have both conditions-and CBT-I helps with the insomnia part.
Why do I feel worse after starting CBT-I?
It’s common, especially during sleep restriction. You’re reducing your time in bed, which creates mild sleep deprivation to rebuild your sleep drive. This causes temporary fatigue and irritability. But it’s a short-term phase. Your body adapts, and within weeks, your sleep becomes deeper and more efficient. This is not a sign it’s not working-it’s a sign it is.


Comments (11)
Daisy L
22 Nov, 2025Oh my GOD, YES. I’ve been screaming this from the rooftops for years! Sleep hygiene is a joke for chronic insomnia-it’s like telling someone with a broken leg to ‘walk more carefully.’ I tried all that crap: lavender oil, weighted blankets, ‘no screens after 9’-and I still lay there like a corpse with anxiety. CBT-I saved my life. Not because it was easy. But because it was real. I cried during sleep restriction week. I wanted to quit. But now? I sleep 7 hours. No pills. No magic. Just science. And yes, I’m still mad at every doctor who told me to ‘relax’.
Anne Nylander
22 Nov, 2025You got this!! I was there too-3am staring at the ceiling, hating my bed. But CBT-I? Totally worked. First week was brutal, like running a marathon with no training. But week 4? I fell asleep in 10 mins. No lie. You’re not broken. You just needed the right tools. Keep going!! You got this!!
Franck Emma
24 Nov, 2025I almost died from this. Not metaphorically. Literally. My heart was racing. My cortisol was through the roof. I thought I was dying every night. Pills? Made me a zombie. CBT-I? It didn’t fix me-it resurrected me.
Eliza Oakes
24 Nov, 2025Oh please. CBT-I is just Big Sleep’s latest scam. You know who profits from this? Pharma. They don’t want you cured-they want you dependent on apps and therapists. Melatonin is natural. Sleep restriction is torture. And who says 7 hours is ‘normal’? I’ve survived on 4.5 for 20 years. My brain is sharper than yours. You’re just scared of your own biology.
Florian Moser
26 Nov, 2025This is the most accurate breakdown of chronic insomnia I’ve ever read. I’ve been through CBT-I twice-once with a therapist, once with Sleepio. Both worked. The first two weeks are brutal, but they’re the price of admission. If you’re reading this and still lying awake, don’t give up. You’re not weak. You’re just in the middle of the hardest part. And it gets better. I promise.
jim cerqua
26 Nov, 2025CBT-I is a cult. They don’t tell you the truth: sleep restriction is just sleep deprivation dressed up as therapy. And those apps? They track your every blink. Who’s selling your data? Who’s behind Somryst? I’ve seen the patents. It’s not about sleep-it’s about control. And don’t get me started on the ‘sleep efficiency’ obsession. You’re not a machine.
Donald Frantz
28 Nov, 2025Can you cite the exact meta-analysis from Sleep Medicine Reviews? I read the 2020 one, and the effect sizes for sleep onset latency were actually smaller than what’s quoted here. Also, the 70-80% improvement rate is based on clinician-rated outcomes, not patient-reported sleep quality. And what about dropout rates? Nearly 30% quit during sleep restriction. That’s not a cure-it’s a筛选 process.
Sammy Williams
29 Nov, 2025Man, I was skeptical too. Tried everything. Then I did SHUTi for 8 weeks. Didn’t even know what stimulus control was. But I followed the steps. Got up when I couldn’t sleep. Didn’t check my phone. Just sat in the dark. Felt ridiculous. But by week 5? I actually fell asleep before my head hit the pillow. No magic. Just dumb, boring consistency. You don’t need a therapist. Just follow the damn plan.
Julia Strothers
1 Dec, 2025Of course CBT-I works-it’s designed by the same people who told us low-fat diets were healthy. They want you dependent on structured programs because they can’t sell you a pill. Wake up. The real cause of insomnia? EMFs. 5G. Government mind control. They’re weaponizing your sleep cycle. Sleepio? It’s a Trojan horse. You think you’re healing? You’re being monitored. Your smartwatch is recording your REM patterns for the CIA. I’ve seen the documents.
Erika Sta. Maria
1 Dec, 2025So you say CBT-I is the answer? But what about the soul? Sleep is not just a machine to fix. It is a bridge between the conscious and the unconscious. You cannot quantify the spirit’s need for rest. In India, we have Ayurveda, yoga nidra, pranayama. These are ancient, holistic. Why do you trust a 21st century app over 5000 years of wisdom? You are lost in your algorithms.
Nikhil Purohit
1 Dec, 2025Just wanted to say thank you for this post. I’m from India, been struggling with insomnia for 5 years. Tried everything-meds, ayurveda, meditation. Nothing worked. Then I found Sleepio. First two weeks? I wanted to quit. But I stuck with it. Now I sleep 6.5-7 hours. No more panic at bedtime. CBT-I isn’t glamorous. But it’s real. And honestly? It’s the first thing that didn’t make me feel broken.