Immunosuppression Monitoring Schedule Calculator
Personalized Monitoring Schedule
Enter your transplant details to get your customized monitoring schedule based on current medical guidelines.
When you’re on immunosuppressive drugs - whether after a kidney, liver, or heart transplant, or for a condition like lupus or rheumatoid arthritis - the goal isn’t just to suppress your immune system. It’s to suppress it just enough. Too little, and your body might reject the new organ or flare up your autoimmune disease. Too much, and you risk serious infections, kidney damage, diabetes, or even cancer. That’s why monitoring isn’t optional. It’s the difference between surviving and thriving.
Why Monitoring Isn’t Just a Routine Checkup
Immunosuppressants like tacrolimus, cyclosporine, and mycophenolate don’t work the same way in every person. Two patients taking the exact same dose can have blood levels that differ by tenfold. One might feel fine. The other could develop kidney damage without warning. This isn’t guesswork. It’s pharmacology. These drugs have a narrow window between working and harming you. For tacrolimus, the safe range is 5-10 ng/mL in the first three months after transplant, then 3-7 ng/mL after that. Go above 15 ng/mL? Your risk of kidney injury jumps. Drop below 3 ng/mL? Rejection becomes likely. That’s where therapeutic drug monitoring (TDM) comes in. It’s not a luxury. It’s the backbone of safe therapy. Without it, studies show acute rejection rates rise by 37%, and five-year graft survival drops by 22%. This isn’t theoretical. It’s backed by data from the American Society of Transplantation. TDM means regular blood tests to measure exactly how much drug is in your system. It’s how doctors adjust your dose before you start feeling sick.Which Drugs Need Monitoring - and How
Not all immunosuppressants need the same level of oversight. Some are predictable. Others are tricky. Cyclosporine and tacrolimus - the most common calcineurin inhibitors - require close TDM. Tacrolimus is usually checked at trough (just before your next dose). Cyclosporine is trickier. Some centers still check just the trough level, but better outcomes come from measuring the C2 level - two hours after your dose. Studies show C2 levels correlate with rejection risk much more strongly than troughs alone. If your C2 is too low, your body might be rejecting the organ. Too high? You’re damaging your kidneys. Sirolimus and everolimus (mTOR inhibitors) are harder to monitor. There’s no clear consensus on the ideal blood level. Some studies suggest 5-10 μg/L, but evidence linking that number to real-world outcomes is weak. The 2022 International Consensus Guidelines even give it a weak recommendation because the data just isn’t strong enough. Still, doctors watch for side effects like high cholesterol, low white blood cell counts, and lung inflammation (pneumonitis). Mycophenolic acid (MPA) - the active part of mycophenolate - is another challenge. Its levels fluctuate because of how your gut and liver process it. Just checking the trough level isn’t enough. The best predictor of success is the AUC - the total amount of drug in your blood over 12 hours. An AUC between 30-60 mg·h/L is linked to 85% rejection-free survival in the first year. But measuring AUC requires five blood draws over a full day. Most clinics can’t do that. So many rely on trough levels, even though they’re less accurate. Corticosteroids like prednisone? No routine blood monitoring needed. But you still need to watch for their side effects: weight gain, high blood sugar, bone thinning, and mood changes. That’s where lab tests and imaging come in.Essential Lab Tests Beyond Drug Levels
Drug levels tell you about the medicine. But your body tells you about the damage. That’s why routine blood tests are non-negotiable.- Full blood count: Mycophenolate and sirolimus can crash your white blood cells, red blood cells, or platelets. A drop in any of these can mean infection risk or bleeding. Check every 1-3 months.
- Creatinine and electrolytes: Cyclosporine and tacrolimus are hard on the kidneys. A 30% rise in creatinine from your baseline is a red flag. Watch for low magnesium - it happens in up to 60% of cyclosporine users and can cause muscle cramps or irregular heartbeats.
- Liver function tests: All these drugs can stress your liver. ALT and AST levels help catch early damage.
- Fasting glucose: Tacrolimus increases diabetes risk by 30% compared to cyclosporine. Monitor every 3-6 months, especially if you’re overweight or have a family history.
- Lipids: Sirolimus and everolimus spike cholesterol and triglycerides in 60-75% of patients. High lipids mean higher heart disease risk. Get tested every six months.
- Calcium, phosphate, uric acid: These help spot bone loss and gout, both common with long-term steroid use.
Imaging: Seeing What Blood Tests Can’t
Some problems don’t show up in a blood tube. That’s where imaging steps in.- Renal ultrasound: Done annually or whenever kidney function changes. It checks for blockages, scarring, or reduced blood flow - all signs of chronic drug toxicity.
- Chest X-ray: If you’re on sirolimus and develop a dry cough or shortness of breath, a chest X-ray can catch pneumonitis early. It’s not perfect - sensitivity is only 70-85% - but it’s fast and cheap.
- Bone density scan (DEXA): Steroids thin your bones. After one year of steroid therapy, get a baseline scan. Repeat every year if you’re still on high doses. Osteoporosis doesn’t hurt until it breaks - and a hip fracture can end your life.
The Future: TTV - Your Body’s Immune Meter
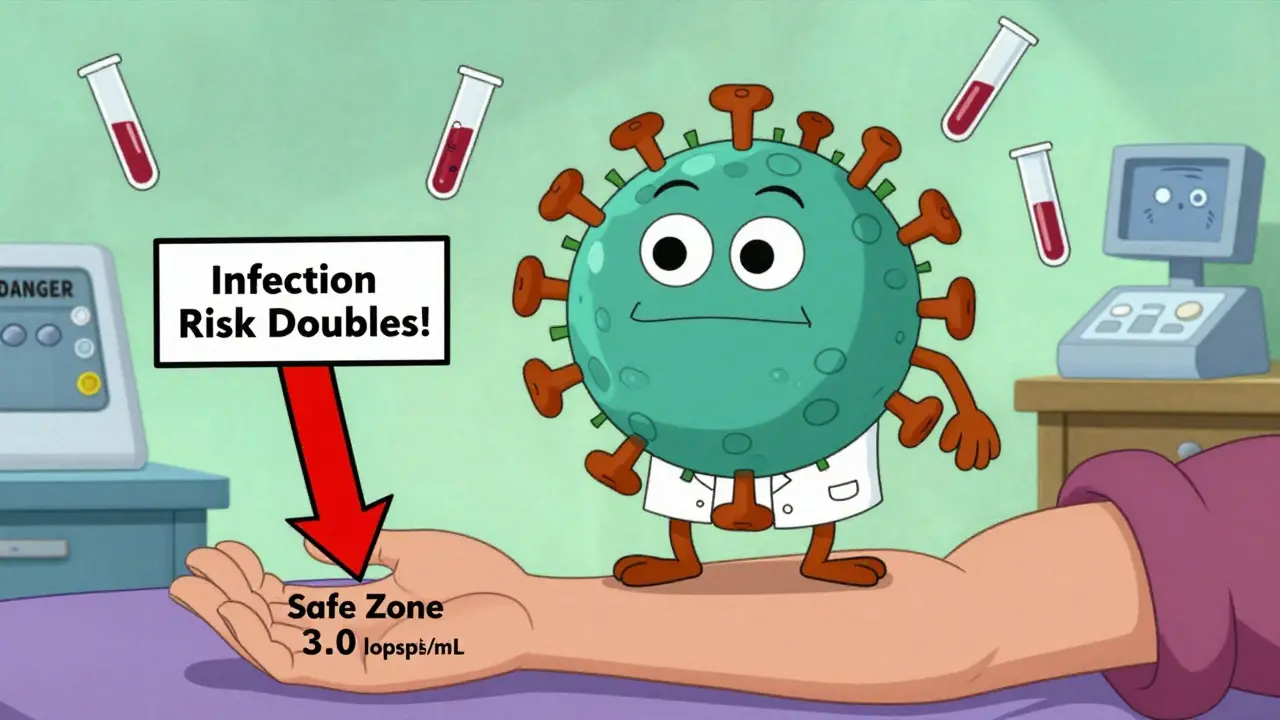
The most exciting development in monitoring isn’t a new drug. It’s a virus you didn’t know you had: Torque Teno Virus (TTV). It’s harmless. It’s everywhere. In healthy people, it’s barely detectable. In transplant patients, it multiplies like crazy - because your immune system is suppressed. Here’s the breakthrough: the amount of TTV in your blood directly reflects how hard your immune system is being suppressed. Too little TTV? Your immune system is still too strong - rejection risk is high. Too much? You’re over-suppressed - infection risk spikes. Studies show the sweet spot for kidney transplant patients between months 4 and 12 is 2.5-3.5 log10 copies/mL. Below 2.5? Your rejection risk triples. Above 3.5? Your infection risk doubles. The TTVguideIT trial, involving nearly 300 patients across the U.S., Europe, and Australia, found that using TTV to guide drug dosing cut infections by 28% and rejections by 22% compared to standard care. It’s not perfect yet. Assays aren’t standardized. Labs don’t all measure it the same way. But the data is strong. The TAOIST trial in France, launching in 2024, will test TTV for long-term monitoring beyond the first year. And by 2025-2026, we may see FDA-approved TTV tests become routine.What’s Holding Monitoring Back?
Despite the evidence, many centers still don’t do it right. A 2022 survey of 150 transplant centers found:- 68% had inconsistent TDM practices between different transplant teams in the same hospital.
- Only 42% had standardized protocols for mycophenolate monitoring.
- 75% said cost was the biggest barrier - LC-MS/MS tests cost $150-$250 each, while cheaper immunoassays can misread levels by 15-20%.
- 63% said reference ranges aren’t standardized. What’s “normal” in one hospital might be dangerous in another.
What’s Next? AI, Point-of-Care Tests, and Less Pain
The future of monitoring is smarter and less invasive. A 2023 study in Nature Medicine used artificial intelligence to predict kidney rejection 14 days before symptoms appeared - by analyzing patterns in tacrolimus levels, TTV load, and creatinine trends. Accuracy? 87%. That’s not science fiction. It’s happening now. Point-of-care devices - think blood test machines you can use in a clinic, not a lab - are in phase 2 trials. FDA approval could come by 2026-2027. Imagine getting your tacrolimus level back in 20 minutes instead of waiting three days. Even more futuristic? Exhaled breath tests to detect drug metabolites. Early lab studies show promise. No needles. Just breathe into a tube.Why This Matters for You
If you’re on immunosuppressants, you’re not just taking pills. You’re managing a delicate balance - one that requires data, not guesswork. Your doctor can’t see inside your body. But blood tests, imaging, and emerging tools like TTV can. The good news? Monitoring works. It saves lives. It keeps organs functioning. It reduces hospital stays and saves money in the long run. A 2022 analysis found that full monitoring costs $2,850 more per year - but prevents $8,400 in rejection and infection-related care. That’s nearly a 3-to-1 return on investment. Don’t skip your labs. Don’t ignore your imaging appointments. Ask your team: What are we monitoring, and why? If they can’t tell you, it’s time to find someone who can.How often should I get blood tests while on immunosuppressants?
In the first year after transplant, expect blood tests every 1-2 weeks initially, then every 2-4 weeks. After the first year, most patients need tests every 1-3 months, depending on stability. If your drug levels or kidney function start to change, your doctor may increase frequency. Always follow your transplant team’s schedule - it’s tailored to your specific drugs and health status.
Can I stop monitoring if I feel fine?
No. Many serious side effects - like kidney damage from tacrolimus or early signs of rejection - don’t cause symptoms until they’re advanced. Feeling fine doesn’t mean your drug levels are safe or your organs are protected. Monitoring catches problems before you feel them. Skipping tests is one of the most common reasons transplant patients lose their grafts.
What’s the difference between immunoassays and LC-MS/MS for drug testing?
Immunoassays are cheaper ($50-$100 per test) and faster, but they can mistake drug metabolites for the actual drug, leading to false readings that are 15-20% off. LC-MS/MS is the gold standard - it identifies the exact drug molecule. It’s more accurate (95-98%) and essential for drugs like tacrolimus and cyclosporine, where small errors can lead to rejection or toxicity. Many centers use immunoassays for routine checks and LC-MS/MS for complex cases or when results are unclear.
Is TTV monitoring available everywhere?
Not yet. TTV testing is still mostly in research centers and large transplant hospitals. It’s not FDA-approved for routine use in the U.S. as of early 2026, but it’s being used in clinical trials and some European centers. Ask your transplant team if they offer it. If they don’t, ask when they plan to - because it’s the next major step in personalized immunosuppression.
Do I need imaging if my blood tests are normal?
Yes. Blood tests show how your body is handling the drugs, but imaging shows structural damage. A normal creatinine level doesn’t rule out early kidney scarring - that’s what a renal ultrasound catches. Steroids can silently thin your bones for years before you break one. A DEXA scan finds that before it’s too late. Imaging complements labs - it doesn’t replace them.


Comments (12)
Katelyn Slack
6 Jan, 2026I just got my first transplant last year and honestly? I was terrified of all the blood tests. But after missing one because I was overwhelmed, my tacrolimus spiked and I ended up in the ER. Now I don't skip a single one. It's not fun, but it's life-saving.
Harshit Kansal
8 Jan, 2026This post is straight fire. I work in a clinic in Mumbai and we dont even have LC-MS/MS machines. We use the cheap immunoassays and pray. Its crazy how much difference accuracy makes.
Vinayak Naik
9 Jan, 2026TTV is the real MVP here. My nephrologist started tracking it last year and it felt like having a secret decoder ring for my immune system. One month my TTV was at 3.8 - we dropped my dose and boom, no more nasty sinus infections. No more feeling like a walking petri dish. This isn't sci-fi - it's science that works.
Kiran Plaha
10 Jan, 2026I'm curious - if TTV is so good, why aren't all hospitals using it? Is it just cost? Or do doctors not trust it yet?
Matt Beck
11 Jan, 2026So... we're basically using a harmless virus as a biological thermostat for our immune system?? 🤯 That's like having a tiny alien inside you whispering, 'Hey bro, you're suppressing too hard.' I'm not mad. I'm impressed. This is the future. And it's weirdly beautiful.
Susan Arlene
11 Jan, 2026I feel like people think if they don't feel sick then they're fine. But your body doesn't scream before it breaks. It just... stops. That's why I do my labs. Even when I'm tired. Even when I'm busy. Even when I don't wanna.
Ashley S
12 Jan, 2026Ugh. More medical bureaucracy. Why can't they just give us the right dose once and leave us alone? I'm tired of being a lab rat.
Jeane Hendrix
13 Jan, 2026I love how this breaks down the why behind each test. As a nurse in oncology, I see patients skip DEXA scans because they think 'it's just bones.' But a hip fracture after steroids? That's not just inconvenient - it's catastrophic. This needs to be shared with every patient I see.
Brian Anaz
15 Jan, 2026We need to stop outsourcing our health to expensive labs. Why can't we just make these tests cheaper? America spends a fortune on this stuff while other countries manage fine with basic blood work. It's not about science - it's about profit.
Cam Jane
15 Jan, 2026You got this. Seriously. I know it feels like a full-time job - the labs, the appointments, the anxiety. But every time you show up, you're choosing life. You're not just taking pills. You're showing up for your future self. And that? That's brave. Keep going. We're rooting for you.
Stuart Shield
16 Jan, 2026The part about TTV gave me chills. A virus that doesn't hurt you, but tells you exactly how hard your body is being suppressed? It's poetic in a weird, scientific way. Like your immune system is whispering secrets through a microscopic messenger. The future is wild.
Amy Le
16 Jan, 2026This is why I hate how fragmented U.S. healthcare is. One hospital uses LC-MS/MS, another uses immunoassays, and they both call it 'tacrolimus level.' How is a patient supposed to know if they're safe? This isn't medicine - it's a mess.