Allergic asthma is the most common form of asthma, affecting about 60% of adults and over 80% of children with asthma in the U.S. It’s not just about wheezing or shortness of breath-it’s your immune system overreacting to everyday things like pollen, dust mites, or cat dander. Unlike non-allergic asthma, which can be triggered by cold air, stress, or exercise, allergic asthma has clear, measurable triggers that can be identified and managed. The good news? When you know what’s setting off your symptoms, you can take real steps to reduce them-sometimes even reduce or eliminate your reliance on inhalers.
What Actually Happens in Your Airways?
When you breathe in an allergen like ragweed pollen or dust mite waste, your body mistakes it for a threat. Special immune cells called mast cells release histamine and other chemicals, causing your airways to swell, tighten, and fill with mucus. This reaction is driven by IgE antibodies, which are elevated in people with allergic asthma-often above 100 kU/L, and sometimes over 400 kU/L in severe cases.
Skin prick tests and blood tests can confirm which allergens are triggering your asthma. A positive skin test shows a raised, itchy bump (wheal) larger than 3mm compared to a control. Sputum tests may show high levels of eosinophils-white blood cells linked to allergic inflammation. If your FeNO (fractional exhaled nitric oxide) is above 25 ppb, that’s another strong sign of type 2 inflammation, which is typical in allergic asthma.
Top Allergen Triggers and When They Strike
Not all allergens are the same. Some are year-round. Others come and go with the seasons.
- Tree pollen: Peaks in March in temperate zones. Levels can hit 10-20 grains per cubic meter. If your asthma flares in early spring, oak, birch, or maple pollen might be the culprit.
- Grass pollen: The biggest summer trigger. June is the worst month, with counts soaring to 50-100 grains/m³. Even mowing the lawn can send you into an attack.
- Ragweed pollen: Starts in August, peaks in September. A single plant can release a billion grains. If your symptoms worsen in late summer, ragweed is likely involved.
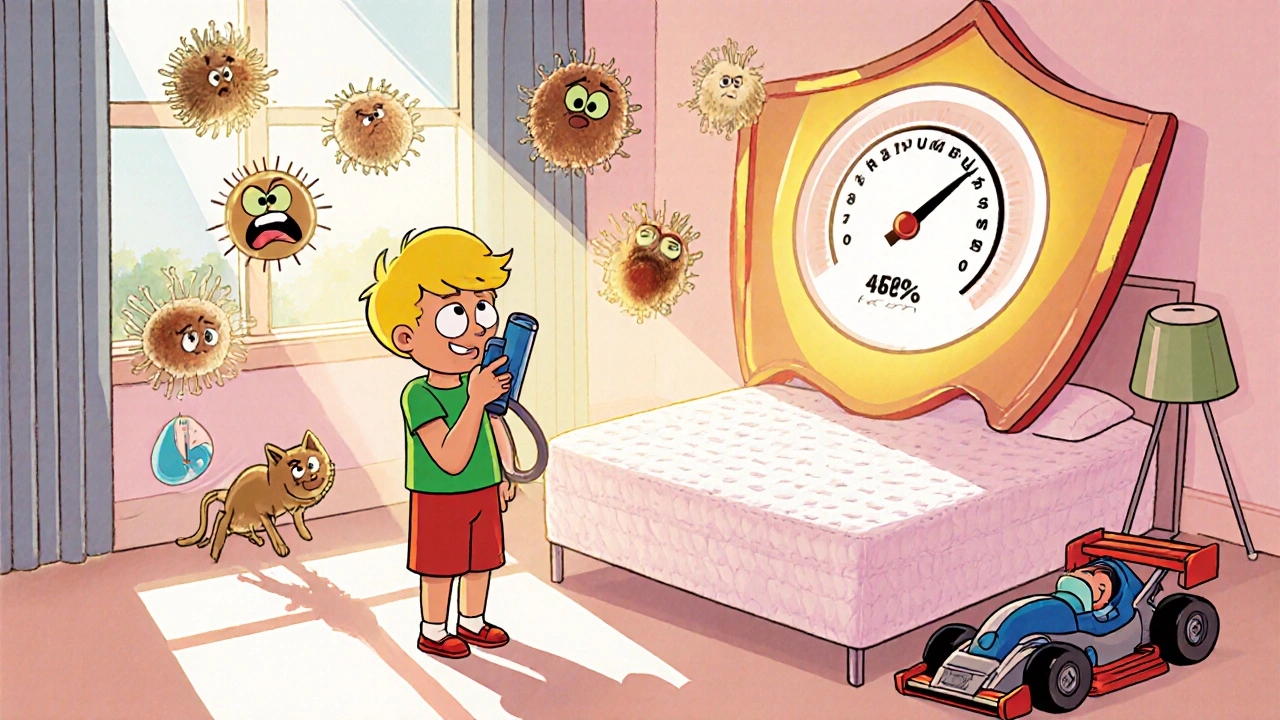
- Dust mites: These microscopic bugs live in bedding, carpets, and upholstered furniture. They thrive where humidity is above 50%. The allergen (Der p 1) reaches dangerous levels-over 2 µg/g of dust-in 84% of U.S. homes. That’s why asthma often gets worse in winter when homes are sealed up and humidifiers are running.
- Cat and dog dander: Cat allergen (Fel d 1) is sticky and lingers for months-even in homes without cats. It’s found in 79% of U.S. homes. Dog allergen (Can f 1) is in 67%. You don’t even need to own a pet; dander travels on clothing and in public spaces.
- Mold spores: Alternaria mold spikes after thunderstorms. When counts go above 500 spores/m³, ER visits for asthma jump 3.5 times. Basements, bathrooms, and leaky windows are common sources.
Real-world data shows that pollen counts above 9.7 grains/m³ can trigger symptoms-even in people on daily medication. That’s why checking local pollen forecasts isn’t optional; it’s part of your daily asthma management.
How to Avoid Allergens (And What Actually Works)
Avoidance sounds simple. But most people try half-measures that don’t work. Here’s what science says actually reduces exposure:
- Bedding: Use allergen-proof covers on mattresses, pillows, and box springs. Look for ones with a pore size under 10 microns. A 2021 study showed this alone can reduce dust mite allergen by 90%.
- Washing: Wash sheets and blankets weekly in water hotter than 130°F. Cold water won’t kill mites. Dry on high heat.
- Vacuuming: Use a vacuum with a HEPA filter. Regular vacuums just blow dust back into the air. Vacuuming twice a week cuts cat allergen by 42%.
- Humidity: Keep indoor humidity between 30-50%. Use a hygrometer to measure it. At 45%, dust mite levels drop from 20 µg/g to just 0.5 µg/g.
- Pollen: Keep windows closed when counts exceed 9.7 grains/m³. Use an air purifier with a HEPA filter in your bedroom. Wear an N95 mask when raking leaves or mowing. Shower and change clothes after being outside-this cuts allergen transfer to bedding by 70%.
- Cats: If you’re allergic and can’t rehome your cat, restrict it to one room (not the bedroom), and bathe it weekly. Use a HEPA filter in the room. Studies show this can reduce airborne Fel d 1 by 50%.
- Mold: Fix leaks immediately. Clean bathrooms with vinegar or bleach. Use exhaust fans. Don’t let houseplants sit in standing water.
One Reddit user with severe dust mite asthma reported their peak flow jumped from 380 to 470 L/min after switching to allergen-proof covers, using a Dyson V15 vacuum, and running a dehumidifier to maintain 45% humidity. That’s not luck-it’s science.

Immunotherapy: The Only Treatment That Changes the Disease
Medications like inhalers and antihistamines treat symptoms. But immunotherapy is the only treatment that can actually change how your immune system responds to allergens.
There are two main types:
- Subcutaneous Immunotherapy (SCIT): Allergy shots. You get weekly injections for 4-6 months, then monthly for 3-5 years. Each shot contains tiny, increasing doses of the allergens you’re sensitive to. Over time, your body learns not to overreact. Studies show 70-80% of patients see major improvement after 12-18 months. The PAT study found that after 3 years, people needed 28% less asthma medication.
- Sublingual Immunotherapy (SLIT): Daily tablets or drops under the tongue. Grastek (for grass) and Odactra (for dust mites) are FDA-approved. It’s less invasive than shots, but you must take it every day. Side effects like mouth itching are common at first-78% of users report it in the first month-but it usually fades.
Research from the Cochrane Review (2021) found that immunotherapy reduces asthma symptoms by 30-50% more than just using inhalers. In one case, a 12-year-old with severe cat allergy reduced their IgE from 120 kU/L to 15 kU/L after three years of immunotherapy-and passed a challenge test without symptoms.
But it’s not for everyone. About 28% of people on shots report injection site reactions. And 35% of SLIT users quit because of persistent oral itching. You need to be committed. Missing doses or stopping early means you lose the benefit.
Who Should Skip Immunotherapy?
Not all asthma is allergic. About 30% of people diagnosed with allergic asthma actually have non-type 2 inflammation-meaning their immune response isn’t driven by IgE or eosinophils. Giving them immunotherapy or expensive biologics like omalizumab won’t help. That’s why testing matters.
If your FeNO is below 25 ppb, your blood eosinophils are under 300 cells/µL, and your skin tests are negative, you likely don’t have allergic asthma. You might need a different approach-like bronchial thermoplasty or macrolide antibiotics, which work better for non-allergic types.
Also, immunotherapy isn’t recommended for people with severe, uncontrolled asthma. You need to get your symptoms stable with medication first. Then, and only then, consider immunotherapy as a long-term solution.

What’s New in 2025?
The field is moving fast. In 2024, the FDA approved CAT-PAD, a new peptide-based immunotherapy for cat allergy that cuts the build-up phase from 6 months to just 8 weeks. A new pollen vaccine (Pollen-VLP) showed 60% symptom reduction with only four doses per year.
Technology is helping too. The Allergen Insight nasal sensor-now FDA-approved-detects airborne allergens as low as 0.1 µg/m³ and sends alerts to your phone. AI platforms like AsthmaIQ use your medication logs, weather data, and pollen counts to predict your next flare-up with 92% accuracy.
And the future? Molecular diagnostics are coming. Testing for specific allergen proteins-like Ara h 8 in birch-pollen sufferers or Alternaria IgE levels above 17.5 kU/L-can now predict who’s at risk for severe reactions. By 2030, we may be able to avoid giving immunotherapy to people who won’t respond, saving thousands in unnecessary costs.
When to See an Allergist
If you’re using your rescue inhaler more than twice a week, waking up at night with asthma symptoms, or missing work or school because of flare-ups, it’s time to see an allergist. They can do the right tests, confirm if your asthma is allergic, and help you decide if immunotherapy is right for you.
Don’t assume your symptoms are just "bad allergies." If you’ve been managing asthma with inhalers alone for years, you might be missing a chance to reduce your dependence on medication-and possibly stop the disease from getting worse.
Allergic asthma isn’t just about avoiding triggers. It’s about retraining your immune system. And with the right plan, you can take back control.
Can allergic asthma go away completely?
In some cases, yes-especially in children. About 50% of kids with allergic asthma see symptoms fade by adulthood, particularly if they avoid triggers and get immunotherapy early. In adults, complete remission is rarer, but long-term immunotherapy (3-5 years) can lead to sustained symptom control even after stopping treatment. Some patients, like the 12-year-old in the AAFA case study, achieve negative challenge tests and near-normal IgE levels after years of therapy.
Are allergy shots worth the time and cost?
For people with confirmed allergic asthma and clear triggers, yes. Medicare covers 80% of the cost in the U.S., with a $18.90 copay per shot in 2024. The average course costs $3,000-$5,000 over 3-5 years. Compare that to $8,000-$12,000 a year for biologics like omalizumab. Plus, immunotherapy reduces inhaler use by up to 40%, lowers ER visits, and improves quality of life. The Cochrane Review found it’s more cost-effective than long-term medication alone.
Can I do allergen avoidance without spending a lot of money?
Absolutely. You don’t need a Dyson vacuum or a $750 dehumidifier to start. Wash bedding weekly in hot water. Use pillowcases and mattress covers made of tightly woven cotton (they’re cheaper than branded ones). Keep windows closed during high pollen days. Use a fan instead of AC to circulate air. Clean bathrooms with vinegar. These steps cost little but can cut allergen levels by 50-90%.
Is immunotherapy safe for kids?
Yes. Both SCIT and SLIT are approved for children as young as 5. SLIT is often preferred for kids because it’s needle-free. The American Academy of Allergy, Asthma & Immunology says it’s safe and effective when started early. In fact, treating allergic asthma in childhood can prevent the progression to more severe asthma and reduce the risk of developing other allergies later.
What if I’m allergic to multiple things?
Immunotherapy can target up to 6 allergens in one mix. Most allergists start with the top 3-4 triggers based on your test results and symptoms. For example, if you’re allergic to dust mites, grass, and cat dander, you’ll get a custom mix. Studies show multi-allergen immunotherapy works just as well as single-allergen treatment. Don’t try to tackle everything at once-focus on the biggest triggers first.
Can air purifiers help with allergic asthma?
Yes, but only if they have a true HEPA filter. Ionizers and UV purifiers don’t remove allergens-they just move them around. A HEPA air purifier in your bedroom can reduce airborne allergens by up to 80%. It’s especially helpful for pollen and pet dander. Place it where you spend the most time, and change the filter every 6-12 months.
Does moving to a different climate help?
Sometimes, but not reliably. Moving to a dry desert area might reduce mold and dust mites, but you could be exposed to new pollens like sagebrush or tumbleweed. Dust mites live everywhere humidity is above 40%, which includes most major cities. Even in places like Phoenix or Las Vegas, indoor allergens remain a problem. Focus on controlling your environment at home instead of relocating.

Comments (10)
robert cardy solano
19 Nov, 2025Been dealing with this since I was 12. Switched to allergen-proof covers and a HEPA filter in my room - my peak flow went from 390 to 480. No joke. I still use my inhaler, but now it’s for emergencies, not daily life. Science works if you actually do the work.
Also, showering after being outside? Game changer. I used to wake up gasping, now I sleep like a baby.
Pawan Jamwal
20 Nov, 2025LOL USA again with their overdiagnosis 😂 We in India have asthma too but we don’t need $750 dehumidifiers or Dyson vacuums. My grandma had asthma for 60 years and she just used neem leaves and kept the house clean. No fancy tech, no shots. Simple living, strong lungs. 😎
Bill Camp
21 Nov, 2025THIS IS WHY AMERICA IS FALLING APART. You people turn EVERYTHING into a medical crisis. You’re allergic to your own shadow now? My grandpa smoked 3 packs a day, never saw a doctor, and lived to 92. You’re not sick - you’re WEAK. Get off the pill mill and breathe like a human.
And immunotherapy? That’s Big Pharma’s new cash cow. They’re selling you hope while charging $5,000 for it. Wake up.
Lemmy Coco
23 Nov, 2025just wanted to say the part about washing sheets in 130f+ water is so true. i used to think cold water was fine... until i started getting night coughs every week. switched to hot wash + high heat dry and boom - no more 3am wheezing. also, i got a $30 cotton mattress cover from amazon and it’s worked just as good as the $120 ones. don’t overthink it.
also, i misspelled ‘washes’ as ‘washes’ in my notes lol
rob lafata
23 Nov, 2025Oh wow, another sanctimonious ‘allergy guru’ post. Let me guess - you also meditate with crystals and only eat organic kale? You think dust mites are your enemy? Nah. Your enemy is your own fucking anxiety. You’ve been conditioned to fear your own home. You don’t need a HEPA filter - you need to stop being a hypochondriac.
And immunotherapy? That’s just your immune system being bullied into submission. They’re literally poisoning you with allergens to ‘train’ it? That’s not science - that’s psychological warfare dressed in white coats. I’ve seen people go from mild wheezing to full-blown anaphylaxis after shots. You’re not curing asthma - you’re turning yourself into a lab rat.
Also, why the fuck is every single recommendation here a $200 product? You want to fix this? Open a window. Let your kids play in the dirt. Stop sterilizing your life. Your immune system doesn’t need a PhD - it needs to be bored.
Matthew McCraney
25 Nov, 2025They’re hiding something. Did you know the CDC admitted in 2021 that pollen counts have been artificially inflated to justify biologic drug sales? And those ‘HEPA filters’? They’re all made in China - same factories that make the masks they told us to wear during the pandemic. You think this is about health? Nah. It’s about control. They want you dependent. They want you buying $750 vacuums and monthly shots. Look at the timeline - asthma rates spiked right after the 2016 FDA approval of SLIT tablets. Coincidence? I think not.
Also, ‘FeNO above 25 ppb’? That’s a number pulled out of a hat. My cousin’s FeNO was 28 and he’s fine. They just need a metric to sell you more meds. Wake up.
And why does every study say ‘studies show’? Name one. Don’t say ‘Cochrane Review’ - that’s just a fancy word for ‘we made it up.’
Rusty Thomas
27 Nov, 2025OMG I JUST REALIZED I’VE BEEN DOING EVERYTHING WRONG 😭 I had a HEPA filter but I never changed the filter for 2 YEARS. And I use my Dyson once a week?? I’m basically a walking allergen factory. I’m going to buy 10 new mattress covers TODAY. Also, I’m banning my cat from the bedroom and I’m crying because I love him so much but I can’t breathe at night 😭😭😭 I’m going to start a support group. #AllergicAsthmaWarrior #HEPAorDie
Sarah Swiatek
28 Nov, 2025It’s funny how we treat asthma like it’s a bug to be eradicated, when really it’s a signal - your body screaming that it’s been overwhelmed. You don’t just ‘avoid triggers’ - you rebuild your relationship with your environment. That’s the real work.
And immunotherapy? It’s not magic. It’s not even ‘training’ your immune system. It’s more like slowly reintroducing your body to the world it was never meant to be shielded from. You’re not curing asthma - you’re learning to live with the fact that you’re part of nature, not separate from it.
But here’s the thing: most people don’t want to do that. They want a pill. A filter. A shot. Something they can buy and forget. But real healing? That’s messy. It’s washing sheets. It’s opening windows in winter. It’s letting your kid play in the dirt. It’s accepting that you’re not in control - and that’s okay.
So yeah. Do the HEPA filter. Do the shots. But don’t forget to breathe. Really breathe. Even if it’s scary.
Dave Wooldridge
29 Nov, 2025They’re putting tracking chips in the immunotherapy vials. I know a guy who got his shot and then his smart fridge started talking to him. He said it asked him, ‘Do you feel better?’ He didn’t even have a smart fridge. That’s not science - that’s surveillance. They’re mapping your immune response to sell ads. You think your asthma is personal? Nah. It’s data. And you’re the product.
Also, ‘AsthmaIQ’? That app tracks your breathing? Yeah, and it’s probably sending your lung data to the government. You think they don’t know who’s allergic? They’ve had your IgE levels since birth. You’re just a walking biometric profile.
Rebecca Cosenza
30 Nov, 2025My mom had asthma. She never used a HEPA filter. She just kept the house clean and stopped buying stuffed animals. I did the same. No shots. No $700 vacuums. Just soap, water, and common sense. You don’t need tech to breathe.
Also, if you’re using your inhaler more than twice a week - you’re not allergic. You’re just lazy.
Fix your life. Not your filter.