Taking a common pain reliever like ibuprofen while on a blood thinner might seem harmless-after all, millions of people do it every day. But what if that combination could double, triple, or even quadruple your risk of internal bleeding? This isn’t a rare side effect. It’s a well-documented, deadly interaction backed by real-world data from over 50,000 patients. If you or someone you know is on a blood thinner and reaches for an NSAID for a headache, arthritis, or back pain, you need to understand the real danger.
What Happens When Blood Thinners Meet NSAIDs?
Blood thinners don’t actually make your blood thinner. They stop it from clotting too easily. That’s critical for people with atrial fibrillation, deep vein thrombosis, or after a heart valve replacement. Common blood thinners include warfarin (Coumadin) and the newer DOACs like apixaban, rivaroxaban, and dabigatran. NSAIDs-like ibuprofen, naproxen, and diclofenac-are anti-inflammatory painkillers. They work by blocking enzymes called COX-1 and COX-2. COX-2 helps with pain and swelling. But COX-1 also protects your stomach lining and helps platelets stick together to stop bleeding. When NSAIDs block COX-1, your stomach gets more vulnerable to ulcers, and your blood can’t clot as well. Now imagine taking both: a blood thinner that slows clotting and an NSAID that further weakens platelet function. It’s like turning off two safety valves at once. The result? A dramatic rise in uncontrolled bleeding.The Numbers Don’t Lie
A major 2024 study from Denmark tracked 51,794 people on blood thinners for venous thromboembolism over 10 years. The findings were alarming:- People taking naproxen had a 4.1 times higher risk of hospitalization for bleeding compared to those on blood thinners alone.
- Diclofenac raised the risk by 3.3 times.
- Ibuprofen, often thought of as the "safer" NSAID, still increased bleeding risk by 1.79 times.
- 2.24 times higher risk of gastrointestinal bleeding
- 3.22 times higher risk of bleeding in the brain
- 1.57 times higher risk of bleeding in the urinary tract
- 1.36 times higher risk of lung bleeding
It Doesn’t Matter Which Blood Thinner You’re On
Many people believe newer blood thinners (DOACs) are safer than warfarin. That’s true in some ways-less monitoring, fewer food interactions. But when it comes to NSAIDs? No difference. The Danish study found the same dangerous spike in bleeding risk whether patients were on warfarin or one of the newer drugs. There’s no "safe" blood thinner to pair with an NSAID. The interaction is class-wide. Even selective COX-2 inhibitors like celecoxib-marketed as "gentler" on the stomach-didn’t reduce the risk. The bleeding danger wasn’t just in the gut. It was systemic.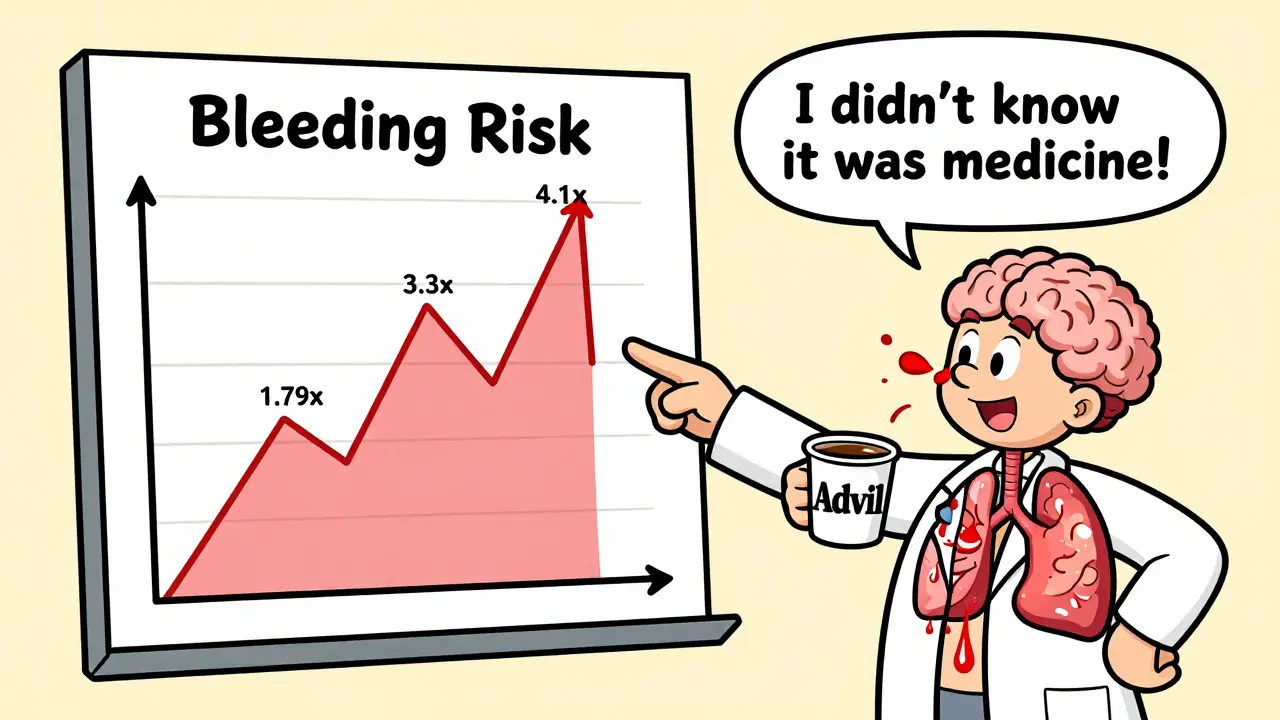
Why People Keep Doing It
It’s not because they’re careless. It’s because they don’t realize NSAIDs are drugs. "I just take Advil for my knee," one patient told a nurse. "It’s not like I’m on medicine." But Advil is ibuprofen. And ibuprofen, even at 200 mg, is enough to interfere with blood thinners. Many patients don’t mention OTC painkillers to their doctors. They think "medication" means prescriptions. But in reality, over-the-counter NSAIDs are responsible for a huge portion of these dangerous interactions. And doctors aren’t always asking. If you’re on a blood thinner, you need to be asked-specifically-about every pain reliever you take. Not just once, but at every visit.What You Should Take Instead
The clear, evidence-backed alternative? Acetaminophen (Tylenol). Unlike NSAIDs, acetaminophen doesn’t affect platelets or stomach lining. It doesn’t increase bleeding risk. It’s the first-line recommendation from the American College of Cardiology for anyone on a blood thinner. But there’s a catch: acetaminophen isn’t anti-inflammatory. So if you have arthritis, gout, or a swollen joint, it won’t reduce the swelling. But it will take the pain away-without putting you at risk. Other options:- Heat or cold packs for joint pain
- Physical therapy to strengthen muscles around painful joints
- Topical creams with menthol or capsaicin
- Low-impact exercise like swimming or walking
What About Stomach Protection?
Some doctors prescribe a proton pump inhibitor (PPI) like omeprazole along with NSAIDs to protect the stomach. But here’s the truth: PPIs don’t fix the problem. They might lower the chance of a stomach ulcer. But they don’t stop bleeding in the brain, lungs, or urinary tract. The Danish study showed that even with a PPI, the overall bleeding risk stayed sky-high. So if you’re on a blood thinner and your doctor says, "Just take a PPI with your ibuprofen," ask: "Is this really safe?" The data says no.
What You Need to Do Now
If you’re on a blood thinner:- Check your medicine cabinet. Do you have ibuprofen, naproxen, or diclofenac? Put them away.
- Review every pain reliever you take-even "natural" ones. Some herbal supplements (like ginger, garlic, ginkgo) also thin blood.
- Ask your doctor or pharmacist: "Is this safe with my blood thinner?" Don’t assume.
- Switch to acetaminophen for pain. It’s the only OTC option with a clean safety record here.
- Keep a list of all medications, including supplements and OTC drugs, and bring it to every appointment.
This Isn’t Just a "Risk"-It’s a Public Health Crisis
In the U.S. alone, about 3 to 6 million people take blood thinners. And over 30 billion OTC ibuprofen tablets are sold every year. That’s millions of people mixing these drugs without knowing the stakes. Hospitals see the results: emergency room visits for internal bleeding, transfusions, ICU stays-all preventable. Health systems are starting to act. Some electronic prescribing systems now flag when a blood thinner and NSAID are prescribed together. But that only catches prescriptions-not the OTC bottles people grab off the shelf. The real fix? Education. Clear, simple, repeated messaging. Not just from doctors, but from pharmacists, nurses, and even pharmacy labels. You don’t need to live in pain. But you do need to choose the right way to manage it.What to Do If You’ve Already Taken Both
If you’ve taken an NSAID while on a blood thinner-even once-don’t panic. But pay attention. Watch for signs of bleeding:- Unusual bruising or purple spots on skin
- Bloody or black, tarry stools
- Bright red blood in urine
- Severe headache, dizziness, vision changes (possible brain bleed)
- Shortness of breath or coughing up blood
- Unexplained fatigue or pale skin (signs of anemia)
Can I take aspirin with a blood thinner?
Aspirin is also an NSAID and inhibits platelets, so combining it with a blood thinner significantly increases bleeding risk. Even low-dose aspirin for heart protection should only be taken with a blood thinner if your doctor specifically recommends it-and even then, the risk is elevated. Never combine them without medical supervision.
Is Tylenol (acetaminophen) really safe with blood thinners?
Yes, acetaminophen is the safest OTC pain reliever for people on blood thinners. It doesn’t affect platelets or the stomach lining. However, don’t exceed 3,000 mg per day, especially if you have liver issues. Always check with your doctor if you’re unsure about dosage.
What if I need an NSAID for a flare-up of arthritis or gout?
If NSAIDs are absolutely necessary-for example, during a severe gout attack-use the lowest effective dose for the shortest time possible, ideally under your doctor’s guidance. Never use them daily. Your doctor may also consider alternatives like corticosteroid injections or colchicine for gout, which don’t carry the same bleeding risk.
Do all NSAIDs carry the same risk?
No. Naproxen carries the highest risk (4.1 times higher), followed by diclofenac (3.3 times), then ibuprofen (1.79 times). But none are safe with blood thinners. Even "milder" NSAIDs still double your bleeding risk. There is no safe NSAID in this combination.
Can I take NSAIDs occasionally if I’m on a DOAC?
Even newer blood thinners (DOACs) don’t protect you from NSAID-related bleeding. The risk is just as high as with warfarin. Occasional use still raises your chance of serious bleeding. The safest choice is to avoid NSAIDs entirely and use acetaminophen instead.

Comments (8)
Harriet Hollingsworth
30 Dec, 2025This is terrifying. I just took ibuprofen last week for my back pain. I’m on warfarin. I didn’t even know this was a thing. My doctor never told me. How many people are dying because we’re all just assuming OTC means harmless? Someone needs to put a warning on every Advil bottle. Like, a skull and crossbones. I’m so mad right now.
I’m telling my mom. She’s 72 and takes naproxen every day for her knees. She’s gonna be furious I didn’t tell her sooner. This isn’t just medical advice-it’s a public service announcement.
Why isn’t the FDA forcing this? Why are pharmacies still selling these together like they’re compatible? I’m starting a petition. Someone help me.
I’m not exaggerating. This could kill someone I love. And nobody’s talking about it.
I’m deleting my ibuprofen from my medicine cabinet right now. And I’m calling my pharmacist. This is life or death.
Thank you for writing this. I’m sharing it with everyone I know.
Chandreson Chandreas
31 Dec, 2025Man… this hits different. 😔
I used to pop ibuprofen like candy after long shifts. Didn’t think twice. Now I’ve got a cousin on DOACs after a stroke. I just asked her if she takes anything for pain-she said ‘yeah, Advil, sometimes.’
I told her to stop. Right then. No debate.
Acetaminophen’s the way. Simple. Safe. No drama. Why do we make health so complicated?
Also-heat packs. I swear by them. Warm towel, 20 mins, feels like a hug for your joints. 🧣
Peace out, NSAIDs. You had a good run. But it’s time to retire.
Thanks for the clarity, OP. You saved someone today.
Kayla Kliphardt
31 Dec, 2025Just wanted to say I’ve been on rivaroxaban for two years. I never took NSAIDs, but I never asked why either. I just assumed Tylenol was the default. I didn’t realize how much I didn’t know.
Thanks for laying this out so clearly. I’m printing this out to show my doctor next visit. I also have a bottle of ginger capsules I’ve been taking for ‘natural inflammation’-I’m going to check if those interact too.
It’s scary how much we’re not told. But also… kind of empowering to know what to look for.
John Chapman
2 Jan, 2026YESSSSSSS!!! 🙌🔥
I’ve been screaming this from the rooftops since my dad almost bled out in the ER last year. He took naproxen for his ‘bad back’ and didn’t tell anyone. He thought it was ‘just a pill.’
HE GOT A TRANSFUSION. HE SPENT A WEEK IN THE ICU. ALL BECAUSE HE THOUGHT ADVIL WAS HARMLESS.
Stop acting like OTC means ‘safe.’ It’s not a candy aisle. It’s a minefield.
Acetaminophen is your friend. Heat packs? Your BFF. Physical therapy? Your soulmate.
And if your doctor says ‘just take a PPI’-tell them to read the Danish study. I dare them.
SHARE THIS. TAG YOUR FAMILY. SAVE A LIFE.
PS: I’m sending this to my entire family group chat. No mercy. 💪
Urvi Patel
4 Jan, 2026You people are so dramatic its pathetic. Everyone knows NSAIDs are risky. You think your grandma doesn’t know ibuprofen is a drug? She’s been taking it for 30 years. She’s fine. Stop acting like this is some groundbreaking revelation. The real problem is you’re scared of everything. Just take the pill. The risk is low. The benefit is high. You’re all overreacting because you watch too many medical documentaries
anggit marga
4 Jan, 2026This is just Western medical fearmongering. In Nigeria we use ginger and pepper for pain and no one dies. You think your pills are better? Look at your hospitals full of people on 12 different drugs. We don’t need your acetaminophen propaganda. Our bodies know better. This study? Probably funded by Big Pharma to sell more Tylenol. I don’t trust your science
Joy Nickles
5 Jan, 2026Okay so I just read this and I’m like… wait wait wait… I’ve been taking naproxen for 5 years?? I’m on Eliquis?? I didn’t know?? My doctor never said anything?? I thought I was being careful?? I’ve been taking it for my migraines?? I’ve had black stools twice?? I thought it was just ‘digestive issues’?? I’m gonna go throw up?? I’m so scared??
Also I think my neighbor’s cat is judging me right now??
Why didn’t anyone tell me?? I’m 34?? I’m supposed to know this??
Also I just googled ‘ginger blood thinner’ and now I’m crying because I take ginger tea every morning??
Can someone just tell me what to do?? I’m not smart enough for this??
Marilyn Ferrera
7 Jan, 2026Acetaminophen is the only safe OTC option. No exceptions.
NSAIDs = increased bleeding risk across all systems. No matter the blood thinner.
PPIs don’t prevent systemic bleeding.
Aspirin is an NSAID. Don’t combine.
Herbal supplements? Many thin blood. Check them.
Physical therapy, heat, cold, movement-effective, safe, sustainable.
Doctors don’t always ask. You must volunteer the information.
This isn’t opinion. It’s data.
Act now. Don’t wait for a crisis.
Share this. Save a life.