IBD Medication Match Calculator
Find Your Best Medication Match
Answer these questions to see which IBD medication might work best for your specific situation. Based on the latest clinical evidence and patient experiences.
Recommended Option
Why this works for you:
Important: This recommendation is based on general principles from clinical evidence. Always consult your gastroenterologist before changing medications.
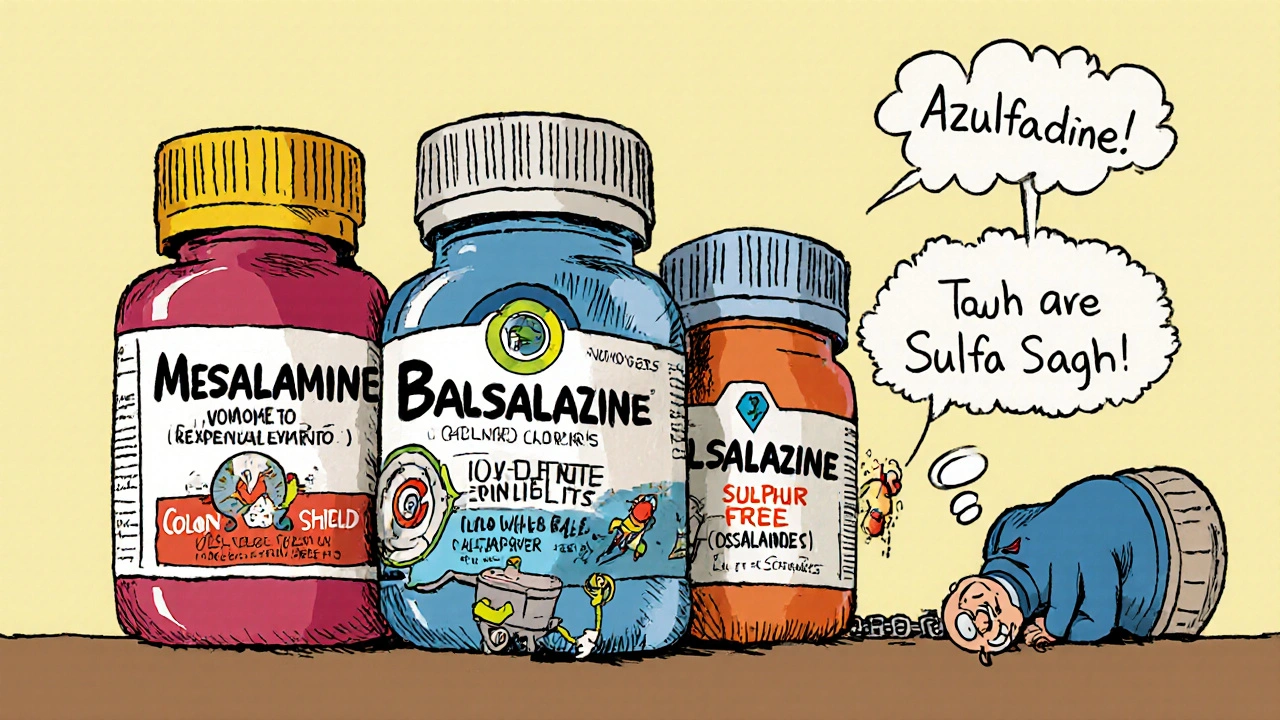
When you’re managing ulcerative colitis or Crohn’s disease, finding the right medication isn’t just about pills-it’s about your daily life. Azulfidine (sulfasalazine) has been around since the 1940s and helped thousands of people control inflammation in their gut. But it’s not the only option anymore. Many patients switch because of side effects, dosing hassles, or lack of results. So what else is out there? And how do the alternatives stack up?
How Azulfidine Works and Why It’s Still Used
Azulfidine is a combination drug: half sulfapyridine, half 5-aminosalicylic acid (5-ASA). It breaks down in the colon, where the 5-ASA part reduces inflammation directly. That’s why it works best for mild to moderate ulcerative colitis affecting the lower intestine.
It’s not fancy, but it’s proven. Studies show about 60% of patients with mild-to-moderate ulcerative colitis see improvement within 4-8 weeks. The American College of Gastroenterology still lists it as a first-line option for some patients, especially those who can’t afford newer drugs.
But here’s the catch: sulfasalazine causes side effects in up to 30% of users. Nausea, headaches, reduced appetite, and dizziness are common. Men may experience temporary infertility. Some people develop rashes or liver enzyme changes. These aren’t rare-many patients quit because of them.
Top Alternatives to Azulfidine
Today, there are several better-tolerated drugs that deliver the same anti-inflammatory punch without the baggage. Here are the most common alternatives.
1. Mesalamine (Asacol, Lialda, Delzicol, Pentasa)
Mesalamine is the purified version of the active part of sulfasalazine-just the 5-ASA, no sulfapyridine. That’s why it’s often called a "cleaner" version.
Studies show mesalamine works just as well as sulfasalazine for inducing remission in ulcerative colitis, but with fewer side effects. In one 2023 trial of 850 patients, 68% of those on mesalamine reported no major side effects compared to only 52% on sulfasalazine.
It comes in different forms: tablets you swallow, capsules that dissolve in the colon, suppositories, and enemas. This flexibility lets doctors tailor treatment to where your inflammation is.
Price-wise, generic mesalamine can cost as little as $50 a month, sometimes less than Azulfidine after insurance.
2. Balsalazide (Colazal)
Balsalazide is another 5-ASA prodrug, designed to release its active ingredient only in the colon. It’s similar to mesalamine but has even less systemic absorption, meaning fewer side effects overall.
In clinical trials, balsalazide showed comparable remission rates to sulfasalazine but with significantly lower rates of nausea and headache. It’s often prescribed when patients can’t tolerate sulfasalazine but don’t need stronger immunosuppressants.
It’s taken three times a day, which can be a hassle, but many patients prefer it because they don’t feel the foggy side effects that come with sulfapyridine.
3. Olsalazine (Dipentum)
Olsalazine is a dimer of 5-ASA, meaning two molecules are linked together. It’s activated only in the colon, so it’s very targeted.
It’s less commonly used than mesalamine or balsalazide, but it’s a solid option for people who’ve had allergic reactions to sulfonamides (like sulfa drugs). Since it contains no sulfur, it avoids the sulfapyridine-related issues entirely.
The downside? It can cause diarrhea in about 20% of users, especially when starting. But that usually improves over time.
4. Biologics (Humira, Remicade, Entyvio)
If you’ve tried 5-ASAs and still have symptoms, your doctor might move you to a biologic. These are injectable or IV drugs that block specific parts of the immune system driving inflammation.
They’re not first-line, but they’re powerful. For example, Humira (adalimumab) helps over 50% of patients with moderate-to-severe ulcerative colitis achieve remission within 8 weeks. They’re used when oral meds fail.
But they come with risks: increased chance of infections, possible reactivation of tuberculosis, and very high costs-often $10,000-$20,000 a year before insurance.
Side-by-Side Comparison
| Drug | Active Ingredient | Dosing Frequency | Common Side Effects | Cost (Monthly, Generic) | Best For |
|---|---|---|---|---|---|
| Azulfidine | Sulfasalazine | 2-4 times daily | Nausea, headache, reduced sperm count, rash | $40-$80 | Low-cost option, mild disease |
| Mesalamine (Asacol, Lialda) | 5-ASA | 1-3 times daily | Abdominal pain, diarrhea, flatulence | $50-$150 | Most patients, preferred first-line |
| Balsalazide (Colazal) | 5-ASA (colon-targeted) | 3 times daily | Headache, upper respiratory infection | $100-$180 | Patients with sulfa allergies |
| Olsalazine (Dipentum) | 5-ASA dimer | 2 times daily | Diarrhea (initial), cramping | $120-$200 | Sulfonamide-allergic patients |
| Humira (Adalimumab) | Anti-TNF biologic | Every other week (injection) | Infection risk, injection site reactions | $800-$1,500 | Severe disease, failed oral meds |
When to Switch from Azulfidine
You don’t need to stay on Azulfidine just because it was your first prescription. Here are clear signs it’s time to talk to your doctor about switching:
- You’re having persistent nausea or headaches that don’t improve after 2 weeks
- You’re trying to get pregnant or your partner is-sulfasalazine can lower sperm count temporarily
- Your symptoms aren’t improving after 8-12 weeks
- You developed a rash, yellowing skin, or dark urine (possible liver issue)
- You can’t afford the out-of-pocket cost, and your insurance doesn’t cover it well
Switching doesn’t mean failure. It just means you’re adapting your treatment to your body’s needs.
What About Natural or Over-the-Counter Options?
Some people turn to probiotics, fish oil, or curcumin (turmeric) supplements hoping to reduce inflammation. While these may help with general gut health, none have been shown to replace prescription 5-ASA drugs in clinical trials.
A 2024 meta-analysis reviewed 17 studies on curcumin and IBD. It found modest symptom improvement in some patients, but no significant remission rates compared to placebo. Probiotics like VSL#3 showed slight benefit in maintaining remission, but not in treating active flares.
Don’t skip your prescribed meds for supplements. Use them as supports, not substitutes.
Real Patient Stories
Mark, 42, was on Azulfidine for 5 years. "I felt like I was constantly sick-not from my colitis, but from the pill. I had constant headaches and couldn’t focus at work. I switched to Lialda and within a month, my energy came back. No more fog. No more nausea. It’s been 3 years and I’m in remission."
Jamila, 28, was diagnosed with ulcerative colitis during her first pregnancy. Her doctor switched her from sulfasalazine to mesalamine because of concerns about fetal safety. "I was scared to change, but mesalamine is pregnancy category B. It’s safe. I delivered a healthy baby."
These aren’t outliers. They’re common outcomes when patients find the right match.

How to Talk to Your Doctor About Switching
Don’t wait until you’re miserable to speak up. Bring these points to your next appointment:
- "I’ve been on Azulfidine for X months. I’m still having [symptoms]."
- "I’m having these side effects: [list them]."
- "I’m concerned about [fertility, cost, long-term use]."
- "What are my options that are easier to tolerate?"
Your doctor should be open to discussing alternatives. Most gastroenterologists have a shortlist of preferred 5-ASA drugs based on patient history, cost, and insurance coverage.
Ask for a copy of your lab results. If your liver enzymes are elevated or your white blood cell count is low, that’s a clear signal to switch.
What If Nothing Works?
If 5-ASAs and biologics don’t help, your doctor may consider other options like immunomodulators (azathioprine, 6-MP), JAK inhibitors (Xeljanz), or even surgery. But that’s rare-over 80% of patients find relief with one of the 5-ASA alternatives.
Don’t give up. Finding the right drug can take time, but it’s worth it. Many people go from feeling constantly unwell to living normally-with fewer pills, fewer side effects, and more energy.
Is sulfasalazine the same as mesalamine?
No. Sulfasalazine is a combination drug made of sulfapyridine and mesalamine (5-ASA). Mesalamine is just the active anti-inflammatory part. Drugs like Asacol or Lialda contain only mesalamine, so they work the same way but with fewer side effects because they don’t include sulfapyridine.
Can I switch from Azulfidine to mesalamine on my own?
No. Never stop or switch medications without talking to your doctor. Even though mesalamine is similar, your body may react differently. Your doctor will help you taper off Azulfidine safely and start the new drug at the right dose to avoid flare-ups.
Does sulfasalazine cause infertility?
In men, sulfasalazine can temporarily reduce sperm count and motility. This effect is reversible-sperm counts return to normal within 2-3 months after stopping the drug. It does not affect female fertility. If you’re trying to conceive, talk to your doctor about switching to mesalamine or another alternative.
Are there generic versions of Azulfidine?
Yes. Generic sulfasalazine is widely available and often costs less than $30 a month with insurance or coupons. However, generic mesalamine products like Asacol HD or Lialda are also available as generics now, and many are priced similarly or lower depending on your plan.
Which alternative is best for someone with a sulfa allergy?
If you have a true sulfa allergy (not just a side effect), avoid sulfasalazine and balsalazide, since they contain sulfonamide components. Olsalazine is the safest 5-ASA option because it contains no sulfur. Mesalamine products like Lialda or Delzicol are also safe-they’re pure 5-ASA with no sulfonamide structure.
How long does it take for alternatives to work?
Most 5-ASA drugs like mesalamine or balsalazide take 2-6 weeks to show full effect. You might feel better in 1-2 weeks, but it takes time for inflammation to fully calm. Biologics like Humira can work faster-some patients see improvement in as little as 2 weeks. Don’t stop early if you don’t feel instant results.
Next Steps
If you’re on Azulfidine and it’s not working for you, you’re not alone. Many people switch successfully. Start by tracking your symptoms and side effects for two weeks. Then schedule a chat with your gastroenterologist. Bring this list of alternatives and ask: "Which one fits my lifestyle, budget, and health goals?"
The goal isn’t just to control your disease-it’s to live well while doing it. There’s a better option out there. You just need to ask for it.


Comments (9)
Brierly Davis
7 Nov, 2025Just switched from Azulfidine to Lialda last month and my life changed. No more headaches, no more brain fog, and I can actually sleep through the night now. Seriously, if you're still on sulfasalazine and it's messing with your head-just talk to your doc. It's not worth suffering for a 1940s drug when there are cleaner options.
Amber O'Sullivan
8 Nov, 2025Azulfidine gave me a rash and made me feel like a zombie why are people still on this
Jim Oliver
9 Nov, 2025Seriously? You're still comparing sulfasalazine to mesalamine? The data is 20 years old. Mesalamine isn't just 'better tolerated'-it's clinically superior in remission rates, bioavailability, and safety profile. If you're still on Azulfidine, you're either underinsured or your GI doesn't read journals.
William Priest
10 Nov, 2025Lialda? Pfft. I'm on the fancy brand name one because the generics are all over the place. My doc says the coating matters. Also, I heard olsalazine tastes like burnt plastic. Who even uses that? #firstworldproblems
Ryan Masuga
11 Nov, 2025I was on Azulfidine for 4 years and thought it was just part of the deal. Then I switched to balsalazide and felt like I got my energy back. Don't give up. Your body deserves a break. Talk to your doctor. You got this.
Jennifer Bedrosian
13 Nov, 2025OMG I switched to mesalamine and now I'm basically a new person like I can go out without planning my life around the bathroom and my partner says I'm not as grumpy anymore?? I'm crying why didn't I do this sooner
Lashonda Rene
14 Nov, 2025I know people say biologics are expensive but I just want to say I was on Humira for a year and it literally saved my life. I was in the hospital three times before that. Yeah it's $1500 a month but I'm not missing my kid's birthday again or having to quit my job because I'm too tired to stand. Insurance fought me but I won. Don't let cost scare you into staying on something that makes you feel awful. You're worth the fight.
Andy Slack
16 Nov, 2025My GI told me to try olsalazine after my sulfa rash. First week I had diarrhea like crazy. Second week? Still weird. Third week? Normal. Now I'm in remission and feel like I finally got my gut back. It's not instant but it works. Don't quit too early.
Rashmi Mohapatra
17 Nov, 2025Ugh why are you all talking about drugs? Just eat turmeric and stop stress. My cousin in Delhi cured her IBD with yoga and no pills. You Americans always think medicine is the answer. You need to detox your soul not your colon.