When a patient walks into your office with a prescription for a brand-name drug, and you know the generic version works just as well and costs a fraction of the price, why don’t you always switch? It’s not because you doubt the science. It’s because you’ve seen what happens when things go wrong - and when they go right.
It’s Not About Quality - It’s About Consistency
Generic medications aren’t cheap imitations. They’re exact copies of brand-name drugs in active ingredients, dosage, and route of administration. The FDA requires them to prove they deliver the same amount of medicine into the bloodstream at the same rate. That’s called bioequivalence - and it’s not a suggestion. It’s a legal requirement. But here’s what most people don’t realize: two generics made by different companies can behave differently in a patient’s body, even if both meet FDA standards. The difference isn’t in the active ingredient. It’s in the fillers, coatings, and how the tablet breaks down. For most drugs - like statins, blood pressure pills, or antibiotics - that doesn’t matter. But for drugs with a narrow therapeutic index, like warfarin, levothyroxine, or epilepsy medications, even small variations can trigger serious consequences. I’ve had patients on lamotrigine for years, stable for months. Then the pharmacy switches them to a new generic. Within weeks, they’re back in the ER with a seizure. Not because the drug didn’t work. Because it worked too differently. When we switched them back to the original brand or a different generic, the seizures stopped. That’s not rare. It’s documented. And it’s why I now write “dispense as written” on prescriptions for antiepileptic drugs, immunosuppressants, and thyroid meds.The Data Doesn’t Lie - But Patients Do
A 2019 JAMA study looked at 10 drugs where both brand and generic versions were available. They tracked hospitalizations, emergency visits, and whether patients kept taking their meds. The results? No meaningful difference in outcomes between brand and generic users. Not for heart meds. Not for antidepressants. Not for diabetes pills. So why do so many patients refuse generics? Because they’ve been told - by ads, by friends, by the internet - that generics are “inferior.” I’ve had patients tell me, “I tried the generic, and I felt weird.” But when I ask what “weird” means, it’s often just fatigue, nausea, or anxiety - side effects they already had on the brand version. The difference? They’re now paying $5 instead of $80, and their brain is looking for a reason to blame the change. The real issue isn’t the drug. It’s the perception. And that’s where education matters more than regulation.What Works: Talking to Patients, Not Just Prescribing
The most effective tool I’ve found? Five minutes. That’s all it takes to explain why a generic is safe. I say: “This pill has the same active ingredient as your brand. It’s made to the same standards. The only difference is the color and the price - and you’ll save $75 a month.” That’s it. No jargon. No FDA citations. Just facts, in plain language. Patients who get that explanation are far more likely to accept the switch. A 2020 study found that 66% of patients were willing to switch if their doctor recommended it. Only 13% did it because the pharmacist suggested it. That tells you who holds the trust. I’ve also started using a simple trick: I hand the patient the generic bottle and say, “This is the same medicine your doctor prescribed. It just doesn’t have the fancy logo.” Then I point to the label: “See this? It says ‘lamotrigine.’ That’s the medicine. The brand name is just the company’s name.” It works. And it saves time later. No calls from panicked patients wondering why their pills look different.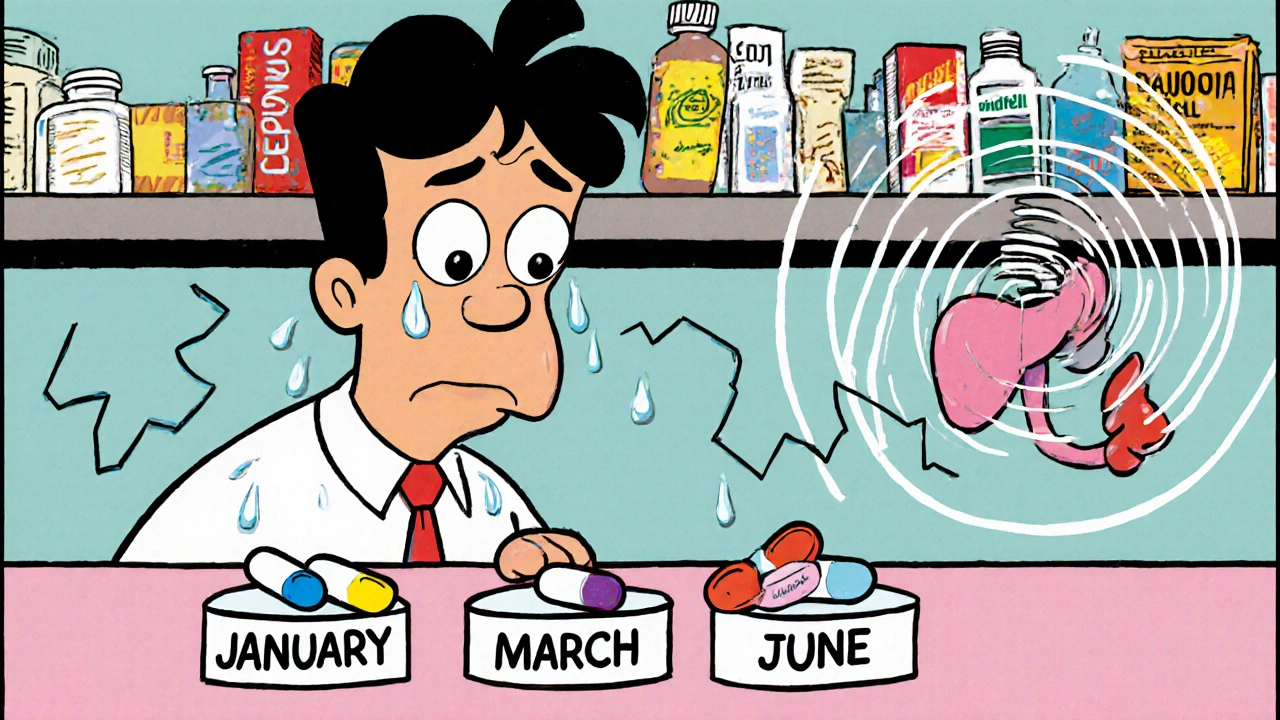
The Hidden Trap: Switching Generics Too Often
Here’s something no one talks about enough: patients don’t just switch from brand to generic. They switch between generics. Insurance companies change preferred manufacturers every few months. Pharmacies stock whatever’s cheapest that week. So a patient on levothyroxine might get one generic in January, another in March, and a third in June. Each switch carries risk. Even if every version meets FDA standards, the body doesn’t always recognize them as the same. I’ve had patients with thyroid levels that swung wildly - not because their dose was wrong, but because they got three different generics in six months. Now I tell patients: “If your pill looks different, call us before you take it.” And I tell pharmacists: “Don’t switch without telling the patient.” Electronic health records now show therapeutic equivalence ratings - AB for safe to substitute, BX for caution needed. But not all systems are connected. Not all pharmacies update in real time. So the burden falls on the provider to stay alert.State Rules Vary - And That Confuses Everyone
In New Zealand, pharmacists can switch generics without asking. In the U.S., it’s a mess. Thirty-one states require pharmacists to notify patients when switching. Twenty-four states don’t protect pharmacists from liability if something goes wrong. Seven states require patient consent before substitution. That means a patient in California might get a generic without knowing. A patient in New York might be asked to sign a form. A patient in Texas might get the brand because the pharmacist is afraid of getting sued. It’s chaotic. And it makes patients distrustful. If one pharmacy switches them and another doesn’t, they assume the system is broken - not that rules are different. I’ve started including a note in every prescription: “Generic substitution permitted unless otherwise indicated.” That way, if a patient is switched without consent, I can point to the prescription and say, “This was your doctor’s intent.”Authorized Generics: The Hidden Middle Ground
There’s a version of generics most people don’t know about: authorized generics. These are the exact same drug as the brand, made by the same company - just sold without the brand name. No different in shape, color, or filler. Just cheaper. I’ve had patients who refused every generic - until I offered them an authorized generic. “This is the same pill as the brand,” I say. “Just no logo.” They take it. No complaints. No side effects. They save $60 a month. The FDA investigated Concerta generics in 2016 after a spike in complaints. Two versions were pulled from the AB rating and downgraded to BX because they didn’t work the same. The authorized generic? No issues. Why? Because it was the same formulation. If you can get an authorized generic, it’s the safest option. Ask your pharmacy. Ask your insurer. It’s not always listed, but it’s often available.
When Generics Save Lives - And Money
Let’s not forget the flip side. I had a patient on atorvastatin. She was 68, on fixed income. The brand cost $120 a month. The generic? $4. She stopped taking it. Her cholesterol soared. She had a mild heart attack. After that, we switched her to generic. She started taking it daily. Her cholesterol dropped. She’s been stable for three years. That’s the real story. For 90% of prescriptions, generics work just as well. They’re not a compromise. They’re the standard. A 2006-2007 Medicaid analysis found that eliminating consent requirements for just three drugs - atorvastatin, clopidogrel, and olanzapine - could have saved over $100 million in a single year. That’s not theoretical. That’s real money. Real lives.What You Can Do Today
- Write “dispense as written” for narrow therapeutic index drugs: antiepileptics, immunosuppressants, thyroid meds, warfarin. - Ask patients if they’ve noticed changes in how their pills look or feel. Don’t assume they’ll tell you. - Know your pharmacy’s generics. If a patient switches and feels off, check if the manufacturer changed. - Use authorized generics when available. They’re the closest thing to the brand - without the price tag. - Explain simply. “Same medicine. Lower cost.” That’s all most patients need to hear. - Track outcomes. If a patient’s lab values or symptoms change after a switch, investigate the generic change first.Generics Aren’t the Problem - The System Is
The science is clear: generics work. For most people, they work just as well as the brand. The problem isn’t the pills. It’s the lack of communication. The patchwork of state laws. The constant switching. The fear. The misinformation. As providers, we’re not just prescribing drugs. We’re managing trust. And when a patient believes their medicine is less effective, it doesn’t matter what the data says. Their body reacts to their belief. The answer isn’t more regulation. It’s better conversations. Start with one patient. Explain why the generic is safe. Watch them relax. Watch them save money. Watch them stay healthy. That’s the real case study.Are generic medications really as effective as brand-name drugs?
Yes, for the vast majority of medications, generics are just as effective. The FDA requires them to have the same active ingredient, strength, dosage form, and route of administration. They must also prove bioequivalence - meaning they deliver the same amount of medicine into the bloodstream at the same rate as the brand. Studies, including a major 2019 JAMA analysis, show no meaningful difference in outcomes for drugs like statins, blood pressure meds, and antidepressants. The only exceptions are narrow therapeutic index drugs like warfarin, levothyroxine, and antiepileptics, where even small variations can matter.
Why do some patients feel worse after switching to a generic?
It’s rarely because the generic is inferior. More often, it’s because the patient’s body is reacting to a change - even if the medicine is the same. The pill might look different, taste different, or have a different filler. For drugs with a narrow therapeutic index, like thyroid meds or seizure drugs, these small changes can affect absorption. Psychological factors also play a role: if a patient believes generics are less effective, they may experience nocebo effects - feeling side effects because they expect them. Always check if the manufacturer changed, not just the brand-to-generic switch.
What are authorized generics, and should I recommend them?
Authorized generics are exact copies of brand-name drugs made by the same company, sold without the brand name. They’re identical in every way - same active ingredient, same fillers, same coating. They’re often cheaper than the brand and more reliable than other generics because they’re made on the same生产线. For patients who refuse generics due to distrust, authorized generics are a perfect middle ground. They’re especially useful for narrow therapeutic index drugs. Ask your pharmacy if one is available - they’re not always listed on formularies, but they’re often in stock.
Can pharmacists switch my prescription to a different generic without telling me?
It depends on your state. In 19 U.S. states, pharmacists can substitute generics automatically. In seven states and Washington, D.C., they must get your consent. Thirty-one states require them to notify you after the switch. Many patients don’t realize their pill changed because the label doesn’t always say “generic.” Always check the label for the manufacturer name. If it’s different from last time, call your provider. You have the right to know.
Should I always ask for the brand-name drug if it’s more effective?
Only if you’ve had a bad reaction to a generic, or if you’re on a drug with a narrow therapeutic index. For most conditions - high blood pressure, cholesterol, diabetes, depression - generics are just as safe and effective. Choosing the brand just because you think it’s better can cost you hundreds a month, and it doesn’t improve your health. If you’re stable on a generic, don’t switch. If you’re not, figure out why - it’s likely the manufacturer, not the generic status.
How do I know if a generic is rated as therapeutically equivalent?
The FDA’s Orange Book lists therapeutic equivalence ratings. Look for “AB” - that means the generic is approved as equivalent to the brand. “BX” means it’s not rated equivalent, often due to inconsistent performance. Some electronic health records show this rating on prescriptions. If you’re unsure, ask your pharmacist or check the FDA’s website. For critical medications, always verify the rating before accepting a switch.
Next steps: If you’re a provider, start documenting your own experiences with generic switches. Track outcomes. Share patterns with your team. If you’re a patient, ask your pharmacist: “Is this the same as last time?” and “Is there an authorized generic?” Knowledge is your best protection.


Comments (15)
Lauren Zableckis
28 Nov, 2025I’ve been prescribing generics for over 15 years and never had a single patient regress because of them. The only time things go sideways is when the pharmacy switches manufacturers without telling anyone. That’s not the drug’s fault-it’s the system’s failure. I tell patients: if the pill looks different, call me. Simple. No drama.
And yes, authorized generics are the secret weapon. I’ve had patients who refused every generic until I handed them the authorized version. Same pill. No logo. They took it without hesitation. Why? Because they trusted it. We need to make that more accessible.
Asha Jijen
28 Nov, 2025generics work fine for me i take them for bp and diabetes no issues at all why do people make it a thing
laura lauraa
29 Nov, 2025Oh, so now we’re blaming the patient’s ‘perception’ for the fact that the FDA’s bioequivalence standards are laughably lenient? Let’s not pretend that ‘fillers and coatings’ are benign. Have you ever seen the list of unregulated excipients in generic tablets? Some contain allergens, dyes, and even carcinogens-none of which are required to be disclosed to patients. And you call that ‘education’? No. That’s negligence dressed up as compassion.
And don’t get me started on ‘authorized generics.’ If the manufacturer can produce an identical product, why aren’t they selling it as the brand? Because they’re profiteering. The system is rigged. You’re not a healer-you’re a corporate apologist.
Darrel Smith
29 Nov, 2025Let me tell you something-this whole generics debate is a national disgrace. I’ve seen patients die because they couldn’t afford their meds, then switched to a cheap generic that didn’t work right, and then they got sicker because they were too scared to speak up. And what do we do? We blame them for feeling ‘weird’? No. We blame the system that lets pharmacies swap pills like baseball cards and calls it ‘cost-saving.’
I had a veteran on warfarin. Got switched to a new generic. INR went from 2.4 to 5.8 in three days. He almost bled out. We didn’t catch it until he showed up in the ER with black stools. That’s not ‘perception.’ That’s a medical emergency. And now I write ‘dispense as written’ on everything that isn’t a vitamin. Because I’m not risking another life on a $3 pill.
Aishwarya Sivaraj
30 Nov, 2025as a nurse in india i see this all the time people think generic means bad but most of the time its the same medicine just cheaper
my mom takes levothyroxine and we always check the maker name on the bottle because last time they switched and her tsh went wild
also authorized generics are a gift from heaven i wish more people knew about them
and yes the system is messed up but talking to patients really helps they just need to hear it in their own language
Iives Perl
2 Dec, 2025the FDA is a puppet. big pharma owns it. authorized generics? that’s a distraction. they’re still made by the same company that gouges you on the brand. the real enemy is the patent system. they’re not letting real competition in. this whole ‘generic’ thing is a scam to make you think you’re saving money while they just rename the pill.
they’re watching you. they know you’ll take it. 🤖
steve stofelano, jr.
3 Dec, 2025It is my sincere belief that the ethical obligation of the healthcare provider extends beyond the mere prescription of pharmaceuticals; it encompasses the cultivation of patient trust through transparent, consistent, and informed communication. The data supporting the therapeutic equivalence of generic medications is robust and well-documented. However, the psychological and sociocultural dimensions of medication adherence cannot be understated. It is incumbent upon clinicians to engage patients in a manner that respects their autonomy while providing unequivocal, evidence-based reassurance. The anecdotal evidence presented herein-particularly regarding the efficacy of plain-language education and the utility of authorized generics-represents a model of compassionate, patient-centered care that ought to be universally adopted.
Jebari Lewis
5 Dec, 2025I’ve been tracking generic switches in my clinic for two years now. We’ve logged over 800 patient transitions. For statins, antidepressants, metformin? Zero clinical impact. For levothyroxine? We saw a 12% spike in TSH fluctuations when pharmacies changed manufacturers without notice. We implemented a protocol: every time a patient gets a new prescription, we check the manufacturer code on the bottle and log it in their chart. Now, if their labs change, we look at the pill first-not the dose. It’s simple, it’s cheap, and it’s saved at least five hospitalizations.
Also-authorized generics are underused. I asked my pharmacy to stock them for all high-risk meds. They said ‘we don’t get many requests.’ That’s the problem. We have to ask. Patients don’t know to ask. We have to lead.
Emma louise
6 Dec, 2025Of course generics work-they’re made in China, India, and other countries where they don’t even have real medical licenses. The FDA lets anything through as long as it’s cheap. You think your ‘authorized generic’ is safe? It’s the same factory, same workers, same standards as the ones that got recalled last year. You’re not protecting patients-you’re enabling a global scam. And you call that ‘education’? It’s propaganda.
Alex Hess
8 Dec, 2025Wow. A 12-page manifesto on generics. How noble. Let me guess-you charge $300 for a 10-minute visit and then lecture patients about ‘perception’ while your clinic’s profit margin on brand-name prescriptions is 400%.
Real talk: most doctors don’t care. They just want the patient to shut up and take the pill. You’re not educating anyone-you’re performing virtue signaling for your peers. And ‘authorized generics’? That’s just a marketing term for ‘we’re still ripping you off, but now it’s legal.’
Leo Adi
8 Dec, 2025In India, generics are the only option for most people. We don’t have the luxury of choosing. And you know what? People live. People thrive. The fear around generics is a Western thing-built on ads and brand loyalty. I’ve seen patients on generics for epilepsy for 10 years. Stable. No seizures. No drama. The real issue isn’t the pill. It’s the narrative. Change the story, change the outcome.
Gaurav Sharma
9 Dec, 2025Let me break this down for you: You’re a doctor. You have authority. You say ‘it’s the same.’ They believe you. But if a pharmacist swaps it without consent, and they feel ‘off,’ they blame YOU. Not the system. Not the pharmacy. YOU. So now you’re the villain. That’s not education. That’s emotional labor you didn’t sign up for.
And don’t get me started on state laws. One state says ‘notify.’ Another says ‘consent.’ Another says ‘no problem.’ Patients don’t care about borders. They just want to feel safe. You’re not fixing the system. You’re just cleaning up the mess.
Shubham Semwal
10 Dec, 2025lol you think patients are dumb for feeling weird after switching? they’re not dumb they’re smart. their body knows something changed. the brand had a certain taste the generic tasted like chalk. that’s not perception that’s biology. and now you want them to trust you because you said ‘same medicine’? nah. show me the batch number. show me the filler list. show me the test results. then maybe i’ll believe you
Sam HardcastleJIV
11 Dec, 2025It is regrettable that the discourse surrounding generic pharmaceuticals has devolved into an emotionally charged, anecdote-driven narrative, rather than one grounded in rigorous pharmacoeconomic analysis and standardized regulatory oversight. The assertion that ‘perception’ drives adverse outcomes is not only reductive, but potentially dangerous. The variability in excipients, dissolution profiles, and bioavailability-however statistically marginal-cannot be dismissed as psychological. A more robust, harmonized global regulatory framework is required, one that mandates full disclosure of all formulation components and prohibits unsupervised substitution without patient consent. Until such time, the current system remains ethically indefensible.
Mira Adam
13 Dec, 2025You talk about ‘five minutes’ like it’s a magic fix. But what about the patient who can’t afford to come back for follow-up labs? What about the one who doesn’t speak English? What about the one whose pharmacy changes the generic every month because of insurance? You’re not solving the problem-you’re putting a Band-Aid on a hemorrhage. And then you pat yourself on the back for being ‘compassionate.’