Psoriasis isn’t just a rash. It’s a lifelong condition that changes how your body works - inside and out. You might see flaky, red patches on your elbows or scalp, but what’s happening beneath the skin is far more complex. Your immune system goes off track, telling skin cells to grow too fast. Instead of taking weeks to replace themselves, they rush to the surface in just a few days. That’s what creates those thick, scaly plaques. And it doesn’t stop at the skin. Psoriasis is tied to heart disease, diabetes, depression, and joint damage. It’s not something you can just ‘scrub off’ or wait out. Managing it means understanding both your skin and your whole body.
What Psoriasis Actually Looks Like - And Where It Shows Up
Most people with psoriasis have plaque psoriasis - the kind with raised, red patches covered in silvery scales. These show up on the knees, elbows, lower back, and scalp. But psoriasis doesn’t stick to one style. Some get guttate psoriasis after a sore throat - small, drop-like spots all over the torso. Others develop inverse psoriasis in skin folds: under the breasts, in the groin, or around the buttocks. These areas are smooth, shiny, and sore, made worse by sweat and friction. Then there’s pustular psoriasis - white pus-filled bumps that can appear suddenly, sometimes with fever. And the rarest form, erythrodermic psoriasis, turns nearly the whole body red and inflamed. It’s dangerous. It can throw off your body temperature and fluid balance. If you see this, you need emergency care.Why Topical Treatments Often Aren’t Enough
Many start with creams and ointments. Calcipotriol (a vitamin D analog) and betamethasone (a steroid) are common. They work well for mild cases. But here’s the problem: applying them twice a day, every day, is hard. People skip doses because it’s messy, time-consuming, or they’re embarrassed. One study found 67% of users don’t stick to their regimen. Even when used correctly, topicals can’t reach deep inflammation. If your plaques cover more than 5% of your skin, or if they’re on your face, nails, or genitals, you need more than creams. That’s when doctors look at phototherapy or systemic drugs.Phototherapy: Light as Medicine
Narrowband UVB light therapy is a proven step up. You go to a clinic 2-3 times a week for 8-12 weeks. The light slows down the overactive skin cells. About 75% of people see major improvement. Some even get home units - but they cost $2,500 to $5,000 upfront. Maintenance runs $100 a month. It’s not cheap, but it’s drug-free and avoids the side effects of pills or injections. Still, it’s not for everyone. People with a history of skin cancer or lupus can’t use it. And it doesn’t fix the immune system - it just calms the skin reaction.Systemic Therapies: When the Whole Body Needs Help
When psoriasis is moderate to severe, you need drugs that work from the inside. Methotrexate, cyclosporine, and acitretin are older options. Methotrexate is taken weekly. It’s effective but can hurt your liver and lower your blood counts. Cyclosporine works fast but can damage your kidneys if used long-term. Acitretin is a vitamin A derivative - great for pustular psoriasis, but risky for women who might get pregnant. These aren’t first choices anymore, but they’re still useful for people who can’t afford biologics or don’t respond to them.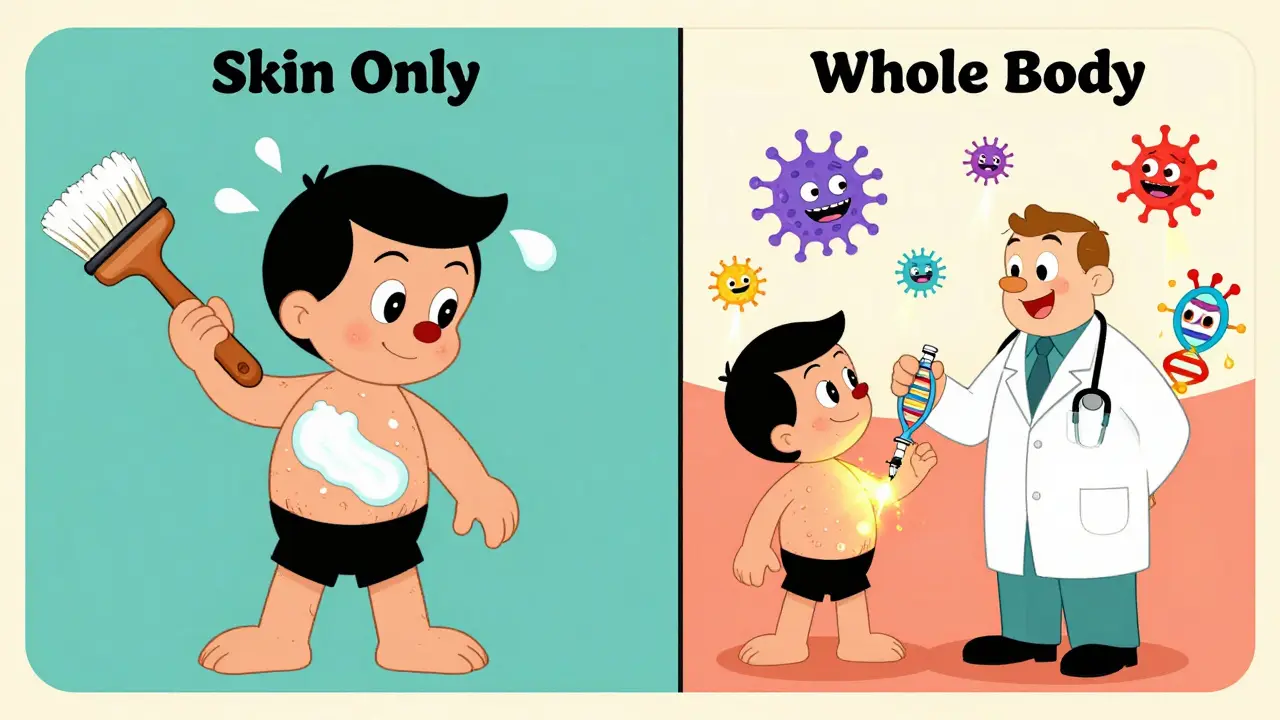
Biologics: Targeting the Root Cause
Biologics are the biggest leap in psoriasis treatment. They’re made from living cells and block specific parts of the immune system that cause inflammation. You get them as injections or infusions, usually every few weeks. There are four main types:- TNF-alpha blockers: Adalimumab (Humira), etanercept - the oldest biologics, still widely used.
- IL-12/23 inhibitors: Ustekinumab - targets two inflammatory signals at once.
- IL-17 inhibitors: Secukinumab, ixekizumab - work fast, often clearing 90% of plaques.
- IL-23 inhibitors: Guselkumab, tildrakizumab - newer, longer-lasting, with fewer injections.
Studies show 50-80% of patients on biologics reach PASI90 - meaning 90% of their plaques disappear. That’s life-changing. On Healthgrades, users rate secukinumab 4.3 out of 5 for effectiveness. But cost is a barrier. Monthly out-of-pocket costs can hit $1,200-$5,500 without good insurance. Many delay treatment because they can’t afford it.
The Hidden Costs: Psoriasis Isn’t Just Skin Deep
Psoriasis isn’t just a skin problem. It’s a systemic disease. People with psoriasis have a 58% higher risk of heart attack before age 50. One in two also has metabolic syndrome - high blood pressure, belly fat, high blood sugar, and bad cholesterol. Depression and anxiety are twice as common. Up to 30% develop psoriatic arthritis - joint pain, stiffness, swelling, often in fingers and toes. That’s why doctors now check your blood pressure, cholesterol, and BMI at every visit. They screen for depression too. If you have psoriasis, your care team needs to include more than a dermatologist. You might need a cardiologist, a rheumatologist, or a therapist.Real-Life Challenges: Adherence, Cost, and Burnout
Even the best treatment fails if you can’t stick with it. People stop biologics because of injections, side effects, or cost. One study found 30-50% quit within a year. Methotrexate causes nausea. Cyclosporine makes you tired. Biologics can increase infection risk - you need a TB test before starting. Some people feel like they’re always managing something. That emotional toll is real. Support groups like MyPsoriasisTeam have over 175,000 users sharing tips and stories. The National Psoriasis Foundation offers free virtual meetings. These aren’t luxuries - they’re lifelines.
What You Can Do Every Day
No treatment works well without daily care. Moisturize. Every day. Thick, petrolatum-based creams or ointments lock in moisture and reduce scaling. Take short, lukewarm showers. Hot water dries you out. Use gentle, fragrance-free cleansers. Avoid scrubbing. Identify your triggers: stress, alcohol, smoking, cold weather, infections. Keep a journal. Some find relief with oatmeal baths or aloe vera. Don’t skip these simple steps - they make your other treatments work better. One UCLA study showed adherence to topical meds jumped 40% when regimens were simplified to once-daily.The Future: Personalized Treatment and New Drugs
The future of psoriasis care is personal. Scientists are looking at your genes to predict which drug will work best for you. Deucravacitinib, a new oral pill approved in 2022, targets a different immune pathway. In trials, 58% of users hit PASI90. It’s taken once a day - no injections. Other oral drugs are in late-stage testing. They could replace biologics for many. But the system isn’t ready. Only 25-30% of people with moderate to severe psoriasis get the right treatment. Rural areas lack dermatologists. Insurance battles delay care. And while biosimilars are coming, they only cut costs by 15-30%. The real win? Getting treatment early. The sooner you control inflammation, the less damage it does to your heart, joints, and mental health.What Success Really Looks Like
The goal isn’t just to reduce plaques. It’s to get to PASI ≤3 (almost no visible disease) and DLQI ≤4 (minimal impact on daily life). That means you can wear shorts, sleep through the night, and not cancel plans because you’re self-conscious. It’s not about perfection. It’s about reclaiming your life. Treatment isn’t one-size-fits-all. What works for your cousin might not work for you. Talk to your doctor. Ask about cost. Ask about side effects. Ask about your heart health. You’re not just treating a rash. You’re protecting your whole body.Is psoriasis curable?
No, psoriasis is not curable with current treatments. But it is highly manageable. Many people achieve near-complete or complete clearance of plaques with the right therapy. The goal is long-term control - minimizing flares and preventing complications like joint damage or heart disease.
Can psoriasis affect my heart?
Yes. Psoriasis is linked to a 58% higher risk of heart attack in people under 50. Chronic inflammation from psoriasis damages blood vessels and increases plaque buildup. Doctors now recommend annual blood pressure checks, cholesterol tests, and BMI monitoring for all psoriasis patients - even if they feel fine.
Why do some treatments stop working over time?
Your immune system can become resistant to some drugs, especially biologics. This is called loss of response. It’s more common with TNF inhibitors. Doctors may switch you to a different class - like from a TNF blocker to an IL-17 or IL-23 inhibitor. Regular check-ins help catch this early.
Are biologics safe for long-term use?
Biologics are generally safe for long-term use when monitored. They increase the risk of infections like tuberculosis or hepatitis, so screening is required before starting. Regular blood tests and check-ups help catch problems early. Most people tolerate them well for years, especially newer IL-23 inhibitors, which have lower infection rates than older biologics.
What’s the best way to apply topical treatments?
Apply a thin layer only to affected areas - not healthy skin. Use it after a shower while skin is still damp to lock in moisture. Don’t rub it in hard. For scalp plaques, use foam or solution forms - they’re easier to apply than creams. If you’re using a steroid, don’t use it for more than 12 weeks without doctor supervision to avoid skin thinning.
Can stress make psoriasis worse?
Yes. Stress is one of the most common triggers. It activates the immune system, which can spark a flare. Managing stress through sleep, exercise, mindfulness, or therapy can reduce flare frequency. Many patients report fewer outbreaks after starting yoga, meditation, or counseling.
Is psoriasis genetic?
Yes. Genetics play a major role - 60-90% of risk comes from inherited factors. If a parent has psoriasis, your chance of getting it is about 10-20%. If both parents have it, that jumps to 50%. But genes alone don’t cause it. You need an environmental trigger - like infection, injury, or stress - to turn on the disease.
Should I avoid sunlight if I have psoriasis?
No - moderate sun exposure often helps. UV light slows skin cell growth. But too much sun burns your skin and raises skin cancer risk. Never use tanning beds. If you’re using photosensitizing drugs like acitretin, avoid sun entirely. Always talk to your doctor before using sunlight as therapy.


Comments (8)
Trevor Davis
14 Jan, 2026Man, I didn’t realize psoriasis was this deep. I thought it was just dry skin until my cousin got diagnosed and started talking about heart risks and depression. Now I check my own elbows every morning like it’s a ritual. It’s wild how something that looks so ‘surface level’ can wreck your whole system.
Thanks for laying this out so clearly. I’m sharing this with my dad-he’s got the plaques on his scalp and refuses to see a specialist. Maybe this’ll finally get him to move.
John Tran
14 Jan, 2026Listen… if you think psoriasis is just a skin thing, you’re living in the 1990s. This isn’t dermatology-it’s immunology with a side of existential dread. The body’s not broken, it’s *betrayed*-by evolution, by stress, by capitalism’s refusal to fund real cures. We’re not patients, we’re canaries in the coal mine of modern life.
And don’t get me started on biologics. They’re like luxury yachts for your immune system while the rest of us are paddling in a leaky canoe made of insurance forms and copays. The real disease isn’t the plaques-it’s the system that makes you choose between rent and your next injection.
Also, typo: ‘PASI90’ should be ‘Pasi-90’ because capitalization is a fascist construct. But I digress. Your article? Deep. Too deep. I cried. I think.
mike swinchoski
15 Jan, 2026You people are making this way too complicated. Just wash your skin. Stop eating sugar. Stop being lazy. I had psoriasis when I was 12 and I cured it by drinking apple cider vinegar and praying every night. No drugs. No shots. Just discipline.
If you’re not willing to change your life, don’t blame the medicine. Blame yourself. And stop acting like you’re some special victim. Everyone gets sick. Not everyone whines about it.
Also, moisturizing? That’s just a scam the drug companies made up to sell lotion. Real men use Vaseline and a towel.
Gregory Parschauer
16 Jan, 2026Let me reframe this: psoriasis isn’t a disease-it’s a systemic biomarker of societal decay. The inflammation? It’s not just in your skin. It’s in your food, your air, your sleep schedule, your LinkedIn feed. Biologics are Band-Aids on a ruptured aorta.
And let’s be real-your dermatologist doesn’t care about your heart. They’re paid per visit, not per outcome. You need a functional medicine practitioner who’ll test your gut microbiome, your cortisol, your heavy metal load. Otherwise, you’re just paying to delay the inevitable.
Also, ‘PASI90’? That’s a marketing metric. Real healing is when you stop checking your reflection before leaving the house. That’s the only cure that matters.
Trevor Whipple
17 Jan, 2026Bro the part about stress making it worse? 100%. I had a flare last year after my dog died. I didn’t even touch my cream for 3 weeks. Then one day I just… started moisturizing again. Didn’t change meds. Didn’t go to the doc. Just started being nice to my skin.
Also, psoriasis on the scalp? Use the foam. Creams are a nightmare. And yeah, UVB works. I did it for 6 months. My wife said I looked like a glowstick. Worth it.
Also, typo: ‘guselkumab’ is spelled with a ‘u’ not an ‘o’. Just sayin’.
Milla Masliy
18 Jan, 2026I’m a nurse in a rural clinic and I see this every day. People come in with plaques covering half their body and say, ‘I can’t afford the biologics.’ Then they ask if they can just use coconut oil and hope for the best.
I hand them free samples. I help them fill out assistance forms. I tell them: ‘Your skin is screaming. Listen.’
And yes-your insurance will fight you. But don’t give up. I’ve seen people go from hiding in hoodies to wearing tank tops in the pool. It’s not magic. It’s persistence.
Also, thank you for mentioning support groups. My patients say MyPsoriasisTeam saved their lives. Not the drugs. The people.
Clay .Haeber
20 Jan, 2026Oh wow. A 2,000-word essay on how to not die from your own immune system. How original. Did you also write a 12-page treatise on why breathing is overrated?
Let me guess-you got your first biologic injection last week and now you’re the Pope of Psoriasis. Congrats. You’re now officially more annoying than your own rash.
Also, ‘PASI90’? That’s not a goal. That’s a TikTok trend. Real people don’t measure their lives in percentage points of skin clearance. They measure it in how many times they forgot they had psoriasis today. That’s the real win.
And for the love of god, stop calling it ‘systemic therapy.’ It’s just expensive shots. We’re not in a sci-fi novel.
Robin Williams
20 Jan, 2026Psoriasis isn’t a battle. It’s a conversation. With your body. With your stress. With your shame. And sometimes… with your doctor if they actually listen.
I used to hate my skin. Now I talk to it. Like, out loud. ‘Hey, you’re doing your best. I’m doing mine.’ It sounds crazy. But it works.
My therapist says trauma lives in the skin. Maybe that’s why the plaques show up when I’m overwhelmed. Not because I’m weak. Because I’m human.
And yeah-biologics saved me. But the real medicine? The oatmeal baths. The walks. The silence. The people who don’t look away when I roll up my sleeves.
You’re not broken. You’re just loud. And the world isn’t ready to hear you. But I am.