Why Generic Drug Knowledge Isn’t Just Important - It’s Life-or-Death
Imagine this: a patient walks into the pharmacy with a prescription for glipizide. The technician grabs what looks like the right pill - but it’s actually glyburide. Same first syllable. Similar shape. Different drug. One treats type 2 diabetes. The other can send blood sugar crashing so low the patient ends up in the ER. This isn’t fiction. It happens. And in 10-15% of medication errors linked to pharmacy technicians, the root cause is confusion between generic and brand names.
Here’s the hard truth: 90% of prescriptions filled in the U.S. are for generic drugs. That means if you’re a pharmacy technician, you’re handling generics every 10 seconds. Not knowing them isn’t a small mistake - it’s a systemic risk. The Pharmacy Technician Certification Board (PTCB), the Department of Veterans Affairs, and state boards don’t just recommend generic drug competency. They require it. And they’re tightening the standards every year.
What Exactly Do You Need to Know? The Official Standards
The PTCB’s 2026 certification exam now dedicates 18% of its content to generic drug knowledge - up from 14% just two years ago. That’s not a minor tweak. It’s a signal: if you can’t confidently tell the difference between metoprolol and metformin, you’re not ready to work in a pharmacy.
Here’s what the standards actually require:
- Know the generic and brand names of at least 200 of the most commonly prescribed drugs
- Recognize drug classifications - like beta-blockers, statins, or SSRI antidepressants
- Understand therapeutic duplication risks - like prescribing two different drugs that do the same thing
- Identify high-alert medications - insulin, anticoagulants, opioids - by name, no exceptions
- Recognize physical characteristics: color, shape, imprint codes
The VA’s standards are even stricter. Technicians managing controlled substances must know 100% of Schedule II-V drugs by both brand and generic name. No guessing. No “I think it’s that one.” One mistake, and it could mean a patient overdoses or a controlled substance gets diverted.
And it’s not just federal. States vary: California requires knowledge of 180 drugs. Texas, only 120. That inconsistency makes it harder for technicians to move between states - and leaves some communities underprotected.
The Cost of Getting It Wrong
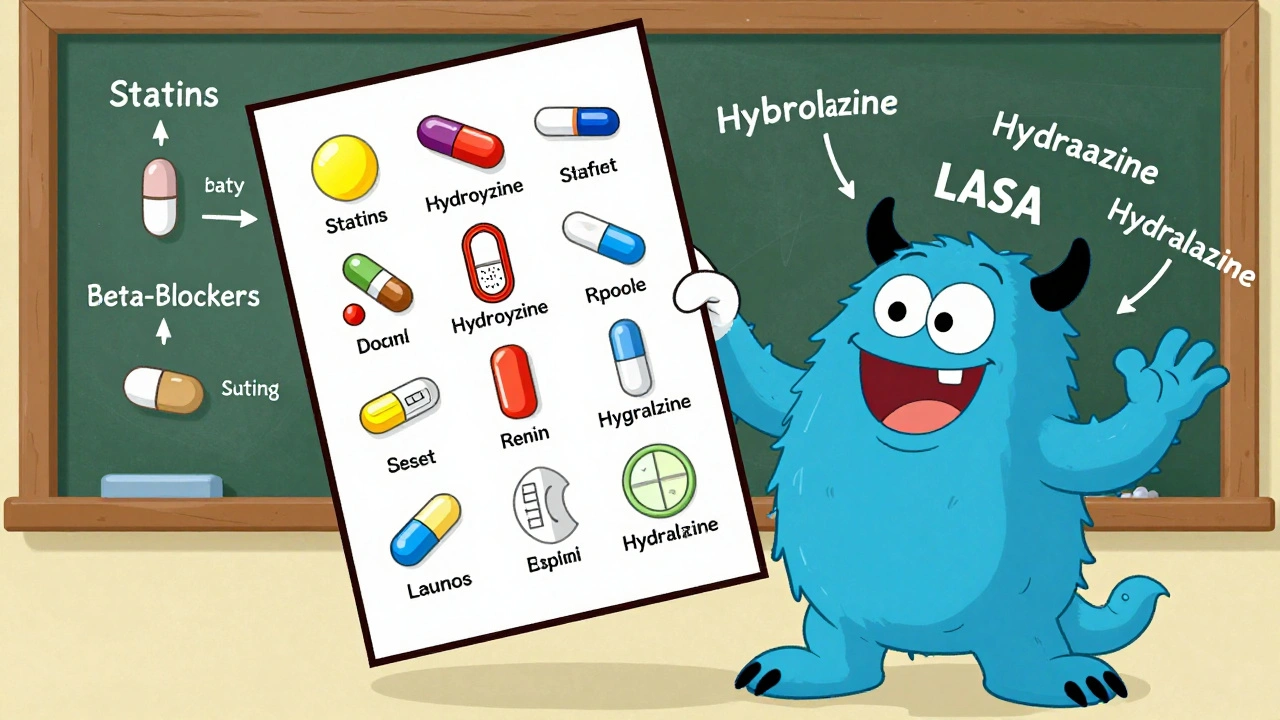
Medication errors kill about 7,000 people in the U.S. every year. The Institute for Safe Medication Practices (ISMP) says 10-15% of those are tied to generic/brand confusion. That’s hundreds of lives lost because someone mixed up hydroxyzine (an antihistamine) with hydralazine (a blood pressure drug).
And it’s not just deaths. A 2023 University of Utah study tracked 1,247 pharmacy technicians across 42 pharmacies. Those who scored below 70% on generic drug tests made 3.2 times more dispensing errors than those who scored above 90%. That’s not a correlation - it’s a direct line from ignorance to harm.
For pharmacies, the financial toll is just as real. A 2023 National Community Pharmacists Association study found that pharmacies where technicians scored over 90% on generic drug tests had 22% fewer dispensing errors. Fewer errors mean fewer lawsuits, fewer insurance claims, and fewer angry patients.
How Do You Actually Learn This Stuff? Real Strategies That Work
Memorizing 200 drug names sounds impossible. But you don’t need to cram them all at once. The most successful technicians use smart, structured methods:
- Group by therapeutic class: Learn all the statins together - atorvastatin, rosuvastatin, simvastatin. Then move to ACE inhibitors. This builds understanding, not just memory.
- Use flashcards with visuals: Apps like RxTechExam or PTCBTestPrep let you match drug images to names. Look at the imprint, the color, the shape. Visual learners find this far more effective than text-only lists.
- Focus on the Top 100 first: These cover over 70% of prescriptions. Master those, then expand to the Top 200.
- Practice daily with real prescriptions: If you’re working in a pharmacy, use downtime to quiz yourself on the day’s most common meds. Write them down. Say them out loud.
One tech on Reddit, ‘GenericGuru,’ said she started grouping drugs by their imprint codes - like a 500 mg metformin tablet has a specific “M 500” stamp. She says it cut her study time in half. Another tech used color-coding: blue pills = blood pressure, green = diabetes, white = antibiotics. Simple. Effective.
And don’t ignore the “look-alike, sound-alike” (LASA) pairs. ISMP lists 37 dangerous combinations. Glipizide vs. glyburide. Clonidine vs. clonazepam. Promethazine vs. propranolol. These aren’t random. They’re traps. Know them. Mark them. Drill them.
What’s Changing - And What’s Coming Next
The game is evolving. In January 2025, the VA started requiring quarterly competency assessments. Technicians must hit 90% accuracy on 100 randomly selected drugs from a 300-item list. Fail twice? You’re pulled from the floor until you retrain.
The PTCB is adding biosimilars to the exam. These are complex, biologic drugs that mimic brand-name biologics like Humira. Their names are longer, weirder - adalimumab-atto, infliximab-dyyb. You can’t memorize them like you do metformin. You need to understand naming conventions: the suffixes, the differences between biosimilars and generics.
And technology is catching up. Walmart rolled out an AI-powered training tool in 2024 that adapts to each technician’s weak spots. It showed a 22% improvement in accuracy and cut onboarding time by 35%. That’s not replacing learning - it’s making it smarter.
But here’s the big question: can we keep up? The FDA approves 15-20 new generic drugs every month. A drug you learned in January might change manufacturers by June. The current system - static lists, annual exams - is already outdated. Experts like Dr. Jerry Fahrni from the University of Minnesota argue we need to shift from memorizing names to understanding drug classes. If you know how a beta-blocker works, you can figure out most of them - even if the name changes.

What This Means for You - Now and in the Future
If you’re training to be a pharmacy technician, generic drug knowledge isn’t just another section on the exam. It’s the foundation of your entire job. You’re not just filling bottles. You’re the last line of defense before a patient takes a pill that could hurt them.
Start now. Don’t wait until the day before your exam. Build a daily habit: one new drug a day. Use flashcards. Test yourself. Talk through it with a coworker. Ask, “Why is this drug in this class?”
If you’re already certified, don’t stop. The standards are rising. The drugs are changing. The stakes are higher than ever. A 2025 survey of 2,315 technicians found that 78% still consider generic drug identification the hardest part of their job - and they’re right. But it’s not because it’s impossible. It’s because most people are trying to memorize without understanding.
Master this, and you’re not just passing an exam. You’re becoming the kind of technician who prevents errors before they happen. Who catches the mix-up. Who says, “Wait - this doesn’t look right.” That’s not just good practice. That’s what saves lives.
Frequently Asked Questions
How many generic drugs must a pharmacy technician know to pass the PTCB exam?
The PTCB expects technicians to be proficient with at least 200 commonly prescribed medications by both generic and brand names. The 2026 exam includes 18% of questions focused on drug identification, with emphasis on the top 200 drugs listed in the PTCB Knowledge Outline. These include high-alert medications like insulin, warfarin, and hydromorphone, where accuracy is critical.
Is generic drug knowledge required in all U.S. states?
Yes. All 50 states now require pharmacy technicians to demonstrate competency in generic drug identification as part of certification or registration. Thirty-two states directly adopt the PTCB certification exam, which includes a dedicated section on generic and brand names. Some states, like California and Utah, have additional state-specific requirements, such as identifying drugs by physical appearance or understanding formulary substitution rules.
What’s the difference between a generic drug and a biosimilar?
A generic drug is a chemically identical copy of a brand-name small-molecule drug - like metformin copying Glucophage. A biosimilar is a highly similar version of a complex biologic drug - like adalimumab-atto copying Humira. Biosimilars aren’t exact copies because they’re made from living cells, not chemicals. Their names include a four-letter suffix to distinguish them (e.g., adalimumab-atto). The PTCB now includes biosimilar naming conventions in its exam as of 2026.
Why do some pharmacy technicians struggle so much with generic names?
Many rely on rote memorization instead of understanding drug classes. With over 200 drugs and 15-20 new generics entering the market each month, memorization becomes unsustainable. The most effective technicians group drugs by function - like all beta-blockers together - and learn patterns in naming (e.g., -olol for beta-blockers, -pril for ACE inhibitors). Visual tools, like imprint and color matching, also help significantly.
How can pharmacies reduce generic drug errors?
Leading pharmacies use a combination of training, technology, and verification. Barcoding systems reduce errors by 89% in hospital settings, but they’re not foolproof - technicians must still recognize when a barcode doesn’t match the drug. Regular competency assessments, quarterly quizzes, and AI-driven learning platforms (like those used by Walmart) have improved accuracy by over 20%. Pairing this with a culture of double-checking high-alert medications makes the biggest difference.


Comments (9)
Brianna Black
9 Dec, 2025This post hits harder than a midnight shift with no coffee. I’ve seen a glyburide/glipizide mix-up firsthand-patient ended up in ICU. We’re not just filling prescriptions; we’re holding lives in our hands. The PTCB upping generic drug weight to 18%? Long overdue. If you’re still memorizing lists without understanding classes, you’re not ready. And yes, I’m talking to you, the tech who says ‘it looks close enough.’
Shubham Mathur
9 Dec, 2025Bro seriously how do you even forget metformin vs metoprolol one is for sugar one is for heart you dont need to be a genius just pay attention
Stacy Tolbert
9 Dec, 2025I used to think I was good until I messed up clonidine and clonazepam. I cried in the supply closet. Not because I got in trouble-because the patient was 82 and just wanted to sleep. That’s when I started using color-coding: blue = BP, green = diabetes, purple = CNS. It’s dumb. It works. I still get nervous every time I touch a new script. And honestly? I think that’s how it should be.
Ronald Ezamaru
10 Dec, 2025There’s a reason the VA requires 100% accuracy on Schedule II-V drugs. It’s not bureaucracy-it’s harm reduction. I trained techs in a rural clinic for five years. The ones who grouped drugs by class-beta-blockers, statins, SSRIs-didn’t just pass the exam. They became the ones other techs asked for help. Memorization fails. Pattern recognition saves lives. And yes, the new biosimilars with those suffixes? They’re not gimmicks. They’re safety features. Learn them.
Ryan Brady
12 Dec, 2025USA has the best pharmacies in the world but now we gotta memorize 200 drugs?? What next, do we need a PhD to hand out Tylenol? My cousin works at a CVS and she just scans the barcode and calls it a day. Maybe if we stopped making everything so complicated, people wouldn’t mess up. Also, why are we even using generics? Brand names are easier.
Raja Herbal
12 Dec, 2025Oh wow, 18% of the exam now? How revolutionary. Meanwhile, in India, we have one tech handling 400 scripts a day with no training, no flashcards, just a prayer and a stapler. You folks worry about glipizide vs glyburide? We worry about whether the pill is even real. But hey, at least your standards are rising. Meanwhile, my cousin’s pharmacy still uses a whiteboard to track insulin. No joke.
Iris Carmen
13 Dec, 2025i just started and honestly the imprint codes are a game changer. like if u see a white oval with 'm 500' u just know its metformin. no thinking needed. i use the rxtechexam app and now i can spot a drug before i even pick it up. also, why is everyone so stressed? its just pills lol
Rich Paul
14 Dec, 2025Let’s be real-this isn’t about memorization, it’s about pharmacokinetic literacy. You don’t need to know every damn drug, you need to understand the structural and functional clusters: -pril for ACEi, -sartan for ARBs, -olol for beta-blockers, -dipine for CCBs. Once you get the suffix logic, you can extrapolate 80% of new generics. The PTCB’s dumbing it down with visual flashcards. Real pros use the naming conventions. Biosimilars? Adalimumab-atto? That’s not a name, it’s a regulatory fingerprint. Learn the pattern, not the product.
Katherine Rodgers
15 Dec, 2025Oh wow, a 22% reduction in errors? Groundbreaking. So let me get this straight-we’ve known for a decade that techs who don’t know their drugs cause harm, but instead of fixing the broken training system, we just make the exam harder? And now we’re adding biosimilars? Cool. Meanwhile, pharmacies still pay techs $15/hour and expect them to memorize 300 drugs like it’s a trivia night. This isn’t education. It’s exploitation with a side of guilt-tripping.