Anticoagulant Dose Adjustment Calculator
Adjust Your Anticoagulant Dose for Rifampin Therapy
This tool estimates the necessary dose adjustments for your anticoagulant medication when taking rifampin. Based on clinical guidelines, rifampin significantly increases drug metabolism, requiring dose changes to maintain therapeutic levels.
When you’re taking rifampin for tuberculosis or to prevent meningitis, you might not think about how it’s quietly changing the way your other medications work. But if you’re also on an anticoagulant like warfarin or a direct oral anticoagulant (DOAC) such as rivaroxaban or apixaban, this interaction isn’t just a footnote-it’s a serious risk. Rifampin doesn’t just kill bacteria. It turns on your body’s drug-processing machinery, and that can drop anticoagulant levels by more than half. The result? A blood clot you didn’t see coming.
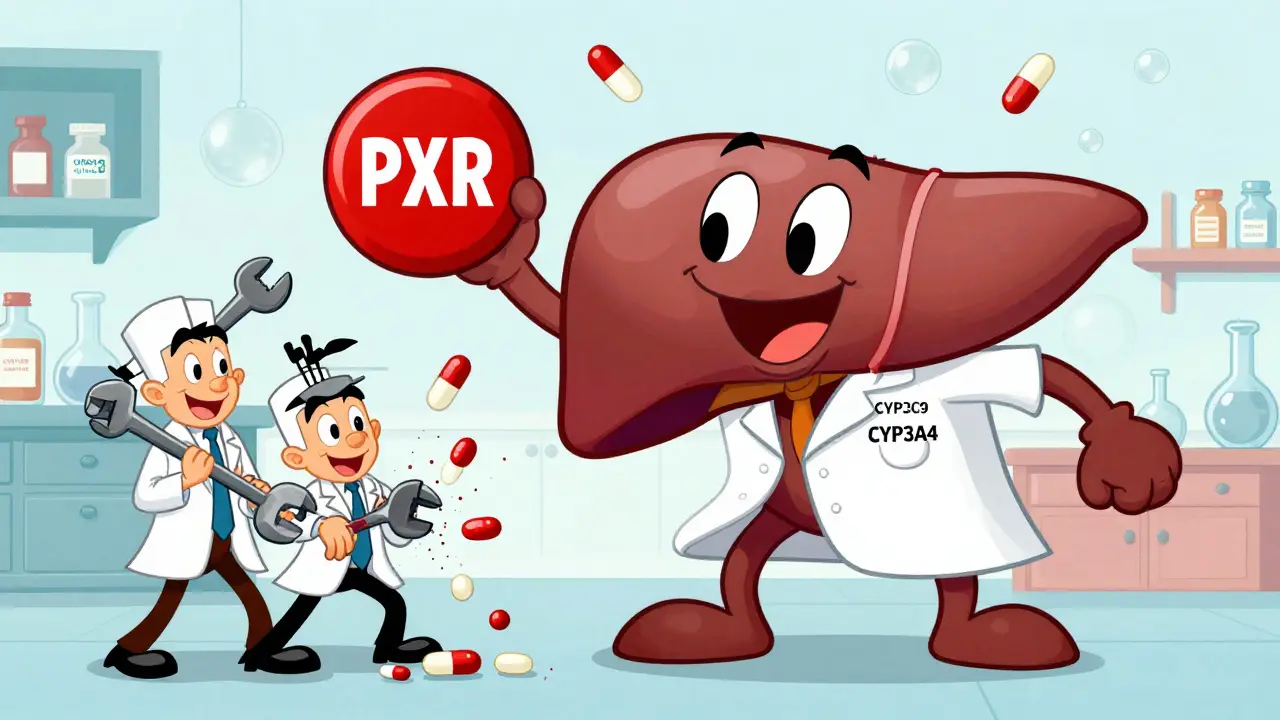
How Rifampin Changes Your Body’s Drug Processing
Rifampin is one of the strongest enzyme inducers known in clinical medicine. It doesn’t block or enhance enzymes directly. Instead, it flips a genetic switch. By activating the pregnane X receptor (PXR) in your liver and intestines, it tells your cells to make more of certain enzymes-especially CYP3A4 and CYP2C9. These enzymes are responsible for breaking down a huge number of drugs, including most anticoagulants and many antivirals.The effect starts within 24 to 48 hours after you take your first rifampin dose. By day five to seven, enzyme levels peak. And here’s the catch: even after you stop rifampin, the effect lingers for two to three weeks. That’s because your body has to degrade all those newly made enzymes before things return to normal. So if you stop rifampin and immediately go back to your old anticoagulant dose, you could end up with dangerously high drug levels and a bleeding risk.
Impact on Vitamin K Anticoagulants (Warfarin, Phenprocoumon)
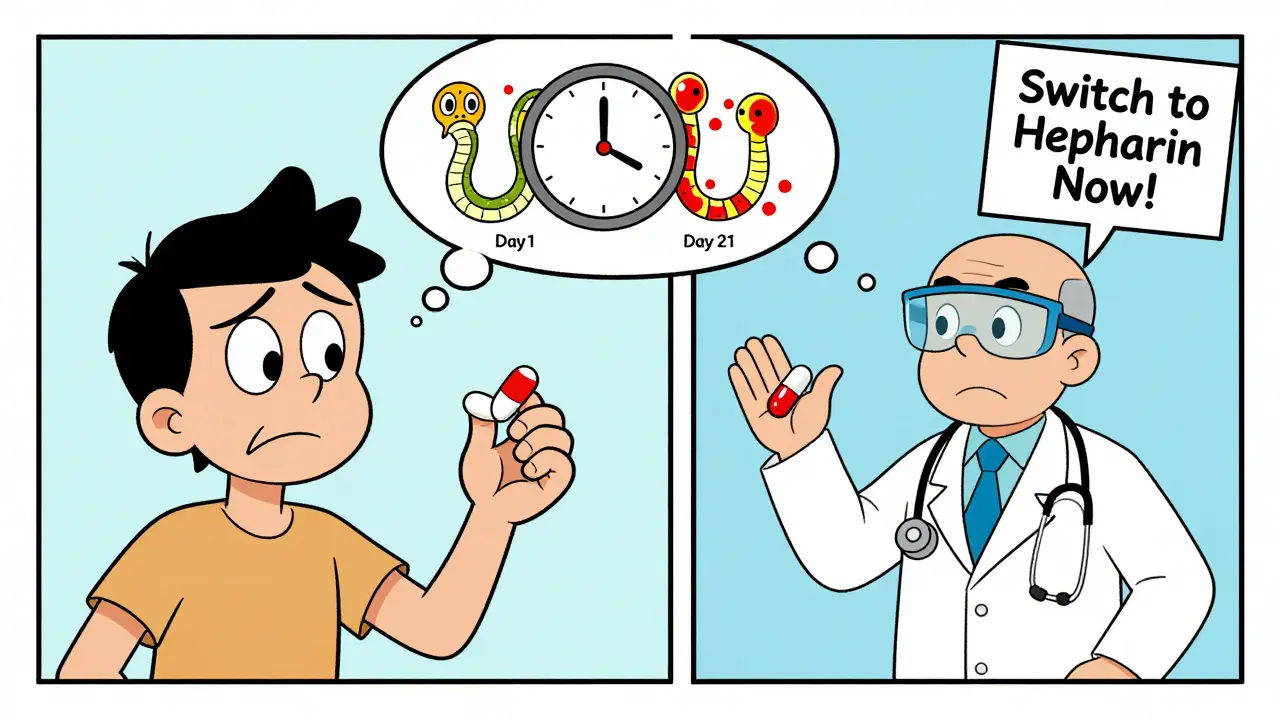
Warfarin has been the go-to anticoagulant for decades, especially for people with mechanical heart valves or atrial fibrillation. But it’s also one of the most vulnerable to rifampin. Studies show that when rifampin is added, warfarin’s blood levels drop by 15% to 74%. That’s not a small fluctuation-it’s enough to make INR values fall out of the therapeutic range.Why does this happen? Warfarin has two active forms: S-warfarin and R-warfarin. S-warfarin is broken down mainly by CYP2C9, the very enzyme rifampin turns up. One study found that S-warfarin levels dropped by up to 60%, while R-warfarin (metabolized by CYP3A4) fell by about 30%. That’s why patients often need to triple or even quadruple their warfarin dose to keep INR stable. One case report described a 57-year-old woman with a mechanical aortic valve. Her INR dropped from 2.8 to 1.2 after starting rifampin-even though she kept taking her usual warfarin dose. She ended up needing heparin injections until 15 days after stopping rifampin, when her INR finally returned to normal.
Direct Oral Anticoagulants (DOACs) Are Also Affected
DOACs like dabigatran, apixaban, rivaroxaban, and edoxaban were supposed to be safer and easier than warfarin. No regular blood tests. Fewer dietary restrictions. But they’re not immune to rifampin. In fact, they’re just as vulnerable.Research shows:
- Dabigatran: 50-60% drop in blood levels
- Apixaban: 50-67% drop
- Rivaroxaban: 50-67% drop
- Edoxaban: 35% drop, but its active metabolites increase slightly
That’s a problem because DOACs have a narrow safety window. Too little, and you get a stroke or pulmonary embolism. Too much, and you bleed internally. Unlike warfarin, there’s no simple test like INR to check if your DOAC level is right. That’s why the European Heart Rhythm Association says concomitant use of DOACs and rifampin “necessitates vigilance and monitoring”-and often recommends avoiding it altogether.
A 2021 study in Frontiers in Pharmacology followed six patients with prosthetic joint infections who needed both rifampin and rivaroxaban. The researchers found that simply increasing the rivaroxaban dose didn’t fix the problem. The timing mattered. Dose changes had to be gradual, with close follow-up, because the enzyme levels didn’t drop immediately after stopping rifampin. Rushing the adjustment could lead to either clotting or bleeding.
Antivirals Are Also at Risk
It’s not just anticoagulants. Rifampin also slashes levels of many antivirals, especially those used for HIV and hepatitis C. Drugs like darunavir, atazanavir, and rilpivirine are metabolized by CYP3A4. When rifampin is added, their blood concentrations can drop by 70% or more. That’s enough to cause treatment failure-and potentially lead to drug-resistant strains of HIV.Even newer antivirals like sofosbuvir (used for hepatitis C) are affected, though to a lesser degree. Studies show that when rifampin is taken with sofosbuvir, sofosbuvir levels drop by about 50%. That’s why the CDC and WHO recommend avoiding rifampin in patients on these regimens unless there’s no alternative-and even then, close monitoring is essential.
What Do Guidelines Say?
The American College of Chest Physicians recommends switching from warfarin to low molecular weight heparin (LMWH) during rifampin therapy. LMWH is injected, not taken orally, and isn’t metabolized by CYP enzymes. That means rifampin doesn’t touch it. Once rifampin is stopped, you can slowly switch back to warfarin over several weeks.For DOACs, the advice is clearer: avoid the combination if possible. But what if you can’t? For example, a patient with atrial fibrillation and active tuberculosis might have no other anticoagulant options. In those cases, the best approach is:
- Switch to LMWH immediately when starting rifampin
- Monitor for signs of clotting (swelling, chest pain, shortness of breath)
- After rifampin is stopped, wait 14-21 days before restarting the DOAC
- Start the DOAC at a reduced dose and titrate up slowly
A 2022 survey of U.S. hospitals found that only 12% had formal protocols for managing rifampin-DOAC interactions. That’s alarming. Most clinicians still don’t know how to handle this. It’s not a rare case-it’s happening more often as DOACs replace warfarin and TB remains a global health issue.
Why This Interaction Is Getting Harder to Manage
There’s a quiet shift happening in anticoagulant use. Between 2010 and 2020, the percentage of patients on DOACs instead of warfarin jumped from 15% to 85%. That’s great for convenience-but worse for interactions. Warfarin at least has INR monitoring. DOACs don’t. So when rifampin drops their levels, you won’t know until it’s too late.And it’s not just anticoagulants. Many antivirals, immunosuppressants, and even some cancer drugs are affected. Rifampin’s broad impact makes it one of the most dangerous drugs to combine with others. Experts call it “one of the most challenging drug interaction scenarios in clinical practice.”

What’s Next? New Drugs Designed to Avoid This
Researchers are already working on solutions. A 2023 study in Nature Scientific Reports looked at milvexian, a new anticoagulant that targets factor XIa instead of thrombin or factor Xa. Early data suggests it’s less affected by CYP3A4 induction. That’s promising. The FDA now requires all new drugs to be tested against strong inducers like rifampin before approval. That’s changing labeling and helping doctors make better choices.Meanwhile, point-of-care INR devices are helping patients on warfarin. These handheld machines are 95% accurate compared to lab tests. They allow patients to check their INR at home and adjust doses quickly when rifampin is added or removed. But again-this only helps with warfarin. For DOACs, we’re still flying blind.
Bottom Line: What You Need to Do
If you’re prescribed rifampin and take any anticoagulant or antiviral:- Don’t assume your current dose is still safe
- Tell your doctor every medication you’re on, including over-the-counter and herbal supplements
- Ask: “Is this drug affected by rifampin?”
- If you’re on a DOAC, expect to switch to heparin injections during rifampin treatment
- After stopping rifampin, wait at least two weeks before restarting your anticoagulant
- Watch for signs of clotting: sudden swelling, chest pain, shortness of breath, dizziness
- Watch for signs of bleeding: unusual bruising, nosebleeds, blood in urine or stool
This isn’t a theoretical risk. It’s a documented, life-threatening interaction that happens more often than most people realize. Rifampin saves lives-but it can also take them if the interaction isn’t managed properly.
Can I just increase my DOAC dose when taking rifampin?
No. Simply increasing the dose of a DOAC like rivaroxaban or apixaban while on rifampin is not safe or reliable. The interaction is unpredictable, and even doubling the dose may not restore therapeutic levels. Studies show that blood levels can still drop by 50% or more despite higher doses. The safest approach is to switch to a non-interacting anticoagulant like low molecular weight heparin during rifampin therapy.
How long does rifampin affect drug levels after I stop taking it?
The enzyme-inducing effects of rifampin can last 2 to 3 weeks after you stop taking it. That’s because your liver needs time to break down the excess CYP3A4 and CYP2C9 enzymes it produced. Restarting anticoagulants too soon after stopping rifampin can lead to dangerously high drug levels and an increased risk of bleeding. Always wait at least 14 days, and preferably 21 days, before resuming your anticoagulant.
Is warfarin safer than DOACs when taking rifampin?
Warfarin is easier to manage with rifampin because you can monitor its effect with regular INR tests. DOACs have no reliable monitoring test, so you won’t know if your levels are too low until you have a clot. For this reason, warfarin is often preferred when rifampin is needed. However, both require dose adjustments. The best option is often to switch to heparin injections during rifampin treatment, regardless of whether you were on warfarin or a DOAC.
Are there any anticoagulants that aren’t affected by rifampin?
Yes. Low molecular weight heparins (like enoxaparin) and unfractionated heparin are not metabolized by liver enzymes and are not affected by rifampin. These are the preferred anticoagulants during rifampin therapy. Newer drugs like milvexian (a factor XIa inhibitor) are being designed to avoid CYP enzyme interactions, but they’re not yet widely available.
Can herbal supplements like St. John’s Wort have the same effect as rifampin?
Yes. St. John’s Wort is also a strong inducer of CYP3A4 and can cause similar drops in anticoagulant and antiviral levels. It’s often overlooked because it’s sold as a supplement, but it’s just as dangerous as rifampin when combined with these drugs. Always tell your doctor about any herbal products you’re taking.
What to Do Next
If you’re currently on rifampin and an anticoagulant or antiviral, don’t wait for symptoms. Contact your doctor or pharmacist right away. Ask for a drug interaction check. If you’re on a DOAC, request a switch to heparin. If you’re on warfarin, schedule more frequent INR checks. This isn’t something to manage on your own. The consequences of getting it wrong are too high.Medication interactions like this aren’t rare mistakes-they’re predictable, preventable, and still happening because many providers aren’t trained to look for them. The more you know, the safer you are. Keep asking questions. Keep tracking your meds. And never assume a drug is safe just because it’s been prescribed.

Comments (12)
Elizabeth Cannon
22 Jan, 2026so i just found out my buddy on warfarin got a clot after starting rifampin for tb... like wtf why is this not common knowledge?? my pharmacist didnt even mention it when i picked up my script. we need better alerts.
siva lingam
23 Jan, 2026rifampin be trippin on everything. next thing you know itll make your coffee taste like regret
Karen Conlin
24 Jan, 2026as someone who’s been on both warfarin and DOACs, this is terrifying. i had no idea rifampin could wipe out my anticoagulant levels like that. my doctor just said ‘take it as usual’ and i believed them. i’m lucky i didn’t have a stroke. if you’re on any of these meds, please, please, please ask about enzyme induction. it’s not just warfarin-it’s everything. even your antivirals. even your supplements. st. john’s wort? yeah, that’s basically rifampin lite. don’t be that person who thinks ‘natural’ means safe. your blood doesn’t care if it’s herbal or pharmaceutical-it just cares if it’s working.
asa MNG
24 Jan, 2026sooo... rifampin is basically the villain in every med thriller?? 😱💀 i mean like... if your meds were a party, rifampin would be the guy who turns off the lights, steals everyone’s snacks, and then says ‘oops’ 🤡💊
Sushrita Chakraborty
26 Jan, 2026This is an exceptionally well-documented and clinically critical interaction. The pharmacokinetic implications of CYP3A4 and CYP2C9 induction are well established in the literature, and the clinical guidelines from the American College of Chest Physicians are unequivocal. The failure of many institutions to implement formal protocols for managing this interaction is a significant gap in patient safety. It is imperative that prescribers receive continuing education on this topic, particularly as DOACs become increasingly prevalent.
Josh McEvoy
27 Jan, 2026they say ‘it’s just TB treatment’... but then your body turns into a drug-eating monster 🤯 i had to go from apixaban to heparin shots... and let me tell you, those needles are the real MVPs right now
Heather McCubbin
28 Jan, 2026they want you to believe this is just science but really it’s the pharmaceutical industry keeping you dependent. why do you think they never warn you? they profit when you get clots and need more drugs. this isn’t medicine-it’s a money machine
Tiffany Wagner
29 Jan, 2026i didn’t know any of this until my mom had to switch to heparin... i’m just glad she’s okay. thanks for posting this, it helped me understand what happened
Helen Leite
29 Jan, 2026the government knows this and lets it happen on purpose. they’re testing how many people will die before they admit the truth. i saw a whistleblower video once…
Shelby Marcel
31 Jan, 2026wait so if i stop rifampin, how long until my blood thinners work again? i’m confused
Karen Conlin
31 Jan, 20262-3 weeks. your liver has to break down all the extra enzymes rifampin tricked it into making. restarting too early = bleeding risk. waiting isn’t optional-it’s life or death.
blackbelt security
1 Feb, 2026if you’re on anticoagulants and get TB, don’t panic. switch to heparin. it’s painful, but it works. this is why we need better drugs. keep fighting for safer options.