What Is Audiometry Testing?
Audiometry testing is the standard way doctors check how well you hear. It’s not a guess or a quick listen-it’s a precise, science-backed process that measures the quietest sounds you can detect at different pitches. These sounds are measured in decibels (dB), and the results are plotted on a graph called an audiogram. This isn’t just about whether you can hear someone talking-it tells your audiologist exactly which frequencies you’re struggling with, and whether the problem lies in your ear canal, middle ear, or inner ear.
The test has been around since the 1940s, built on the Hughson-Westlake method, and today it’s the gold standard used by clinics, hospitals, and hearing centers worldwide. The American Speech-Language-Hearing Association (ASHA) and the World Health Organization both agree: if you need to know the real state of your hearing, audiometry is the only test that gives you clear, repeatable numbers.
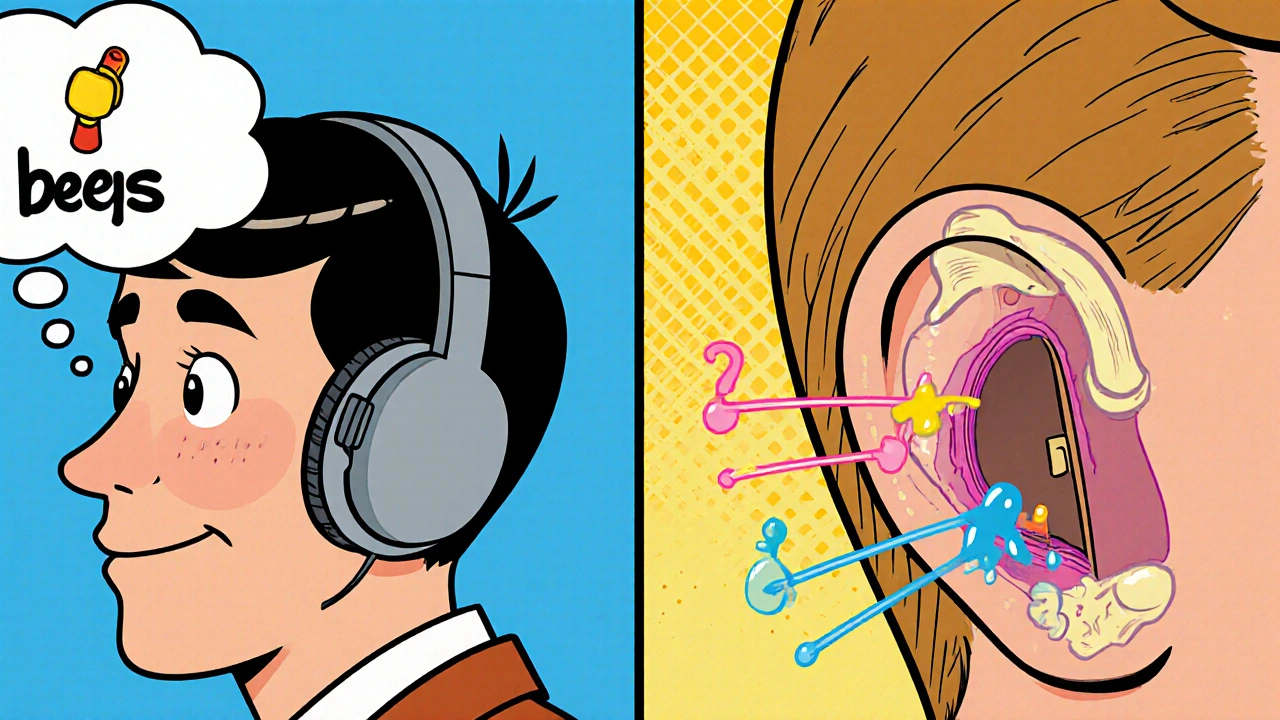
How Does It Work? Air vs. Bone Conduction
There are two main parts to a full audiometry test: air conduction and bone conduction. In air conduction, you wear headphones, and tones at different pitches-like a beep from a low rumble to a high whistle-are played at varying volumes. You signal when you hear each one, usually by pressing a button or raising your hand.
Bone conduction is different. A small device called a bone oscillator is placed behind your ear, on the mastoid bone. It sends sound vibrations straight to your inner ear, skipping your eardrum and middle ear. If your bone conduction results are better than your air conduction results, that means something’s blocking sound in your outer or middle ear-like wax, fluid, or a damaged eardrum. This is called conductive hearing loss.
If both air and bone conduction show the same level of hearing loss, the problem is in your inner ear or auditory nerve. That’s sensorineural hearing loss, the most common type, often caused by aging, noise exposure, or genetics.
Decibel Levels Explained: What Do the Numbers Mean?
Decibels (dB) measure loudness. But in hearing tests, they’re not about how loud a sound is in the world-they’re about how loud it needs to be for you to hear it. The scale is set so that 0 dB HL (hearing level) is the quietest sound a healthy young adult can detect.
Here’s what the numbers actually mean:
- 0-25 dB HL: Normal hearing. You hear whispers, rustling leaves, and ticking clocks without effort.
- 26-40 dB HL: Mild hearing loss. You miss soft speech, especially in noisy rooms. Consonants like ‘s’, ‘t’, and ‘k’ become fuzzy.
- 41-55 dB HL: Moderate hearing loss. You struggle to follow conversations, even one-on-one. You might turn up the TV too loud.
- 56-70 dB HL: Moderately severe hearing loss. You need people to speak slowly and clearly. Group chats are hard.
- 71-90 dB HL: Severe hearing loss. You hear loud sounds but miss most speech. Hearing aids are essential.
- 91+ dB HL: Profound hearing loss. You may only feel vibrations. Cochlear implants are often considered.
Most people don’t realize that hearing loss doesn’t happen all at once. It usually starts in the higher frequencies-around 3,000 to 6,000 Hz-where consonants live. That’s why you might say, “I can hear people talking, but I can’t understand what they’re saying.” That’s not your fault. It’s your audiogram showing the problem.
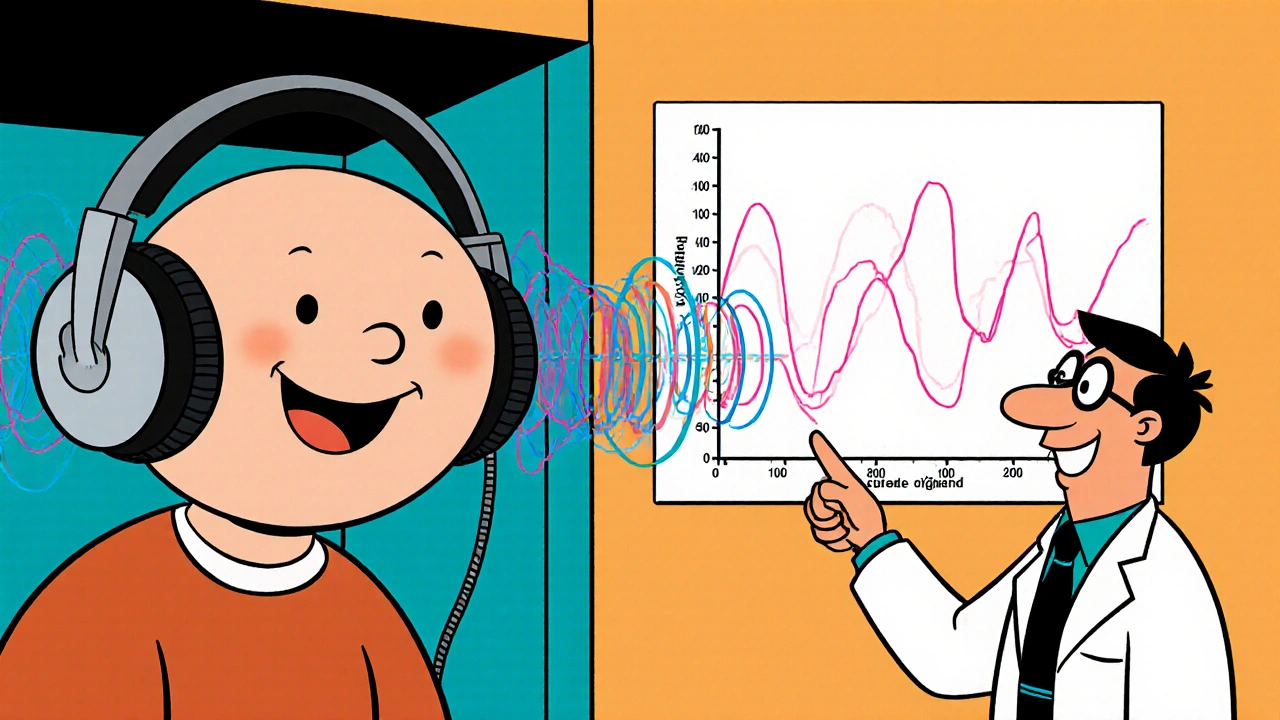
Speech Testing: More Than Just Beeps
Audiometry isn’t just about tones. After the pure-tone test, you’ll do speech testing. You’ll hear words like “cat,” “boat,” or “sun” played at different volumes. The audiologist finds the lowest level where you can repeat 50% of the words correctly-that’s your Speech Reception Threshold (SRT).
Then comes the real test: speech discrimination. You hear the same words at a louder level, and you’re asked to repeat them. If you score below 80%, it means your brain is having trouble processing sound, even when it’s loud enough. This often happens with nerve damage or conditions like auditory processing disorder.
Some people have normal pure-tone results but terrible speech scores. That’s a red flag. It could mean a tumor on the hearing nerve, or early signs of neurological issues. That’s why speech testing isn’t optional-it’s critical.
Tympanometry and Other Supporting Tests
Audiometry doesn’t stop at sound. Tympanometry checks how your eardrum moves. A small probe is placed in your ear, and air pressure changes while a tone plays. The machine measures how well your eardrum responds. A flat line (Type B tympanogram) means fluid is behind your eardrum-common in ear infections, especially in kids.
For babies, toddlers, or people who can’t respond reliably, doctors use visual reinforcement audiometry. Kids get rewarded with a spinning toy or light when they turn toward a sound. It turns a medical test into a game.
For newborns, the CDC recommends a hearing screen before leaving the hospital. If they fail, they get a full diagnostic audiometry by three months old. Early detection means early intervention-critical for language development.
What to Expect During the Test
You’ll sit in a quiet, soundproof booth. You’ll wear headphones or earplugs. You’ll hear beeps, clicks, and spoken words. You’ll press a button when you hear something. It’s simple. But it’s not fast. A full diagnostic test takes 30 to 45 minutes.
Some people find the bone oscillator uncomfortable, especially if they wear glasses. The device presses gently against the bone behind the ear. It’s not painful, but it can feel strange.
Don’t be afraid to ask questions. If you don’t understand why they’re testing bone conduction or what the audiogram means, ask. A good audiologist will explain your results using your audiogram like a map-showing you exactly where your hearing drops off.
Who Needs Audiometry Testing?
You don’t need to wait until you’re struggling to get tested. Here’s who should consider it:
- People over 50-about 25% have hearing loss by age 65.
- Those exposed to loud noise at work or hobbies-construction, music, hunting, lawn equipment.
- People with a family history of hearing loss.
- Anyone who says, “Everyone mumbles,” or “I need the TV louder than before.”
- Patients on ototoxic medications like certain antibiotics or chemotherapy drugs.
- Children with delayed speech or frequent ear infections.
Many people think hearing loss is just part of aging. But it’s not. It’s a medical condition-and one that can be managed. The sooner you know, the sooner you can protect your hearing and your communication.
Common Misconceptions
Some think retail hearing aids or phone apps can replace a professional test. They can’t. Phone apps aren’t calibrated to medical standards. Retail screenings might catch major loss, but they miss the subtle, early changes that matter most.
Others believe if you can hear loud sounds, you’re fine. But hearing loss often starts in the high frequencies, where speech clarity lives. You might hear a dog bark but miss the ‘s’ in “sun.”
And no, hearing aids don’t fix everything. They amplify sound, but if your brain can’t process it, you still won’t understand speech. That’s why speech testing is part of the full picture.
What Happens After the Test?
Your audiologist will show you your audiogram. They’ll explain what each line means. They’ll tell you if you have conductive, sensorineural, or mixed hearing loss. They’ll tell you if you’re a candidate for hearing aids, and which type would suit your lifestyle.
If you need hearing aids, they’ll match them to your audiogram-not just your budget. Modern hearing aids can be programmed to boost only the frequencies you’re missing. That’s personalized hearing.
For some, the next step is a referral to an ENT doctor, especially if there’s a sudden drop in hearing, ringing in the ears, or dizziness. Audiometry doesn’t diagnose everything-but it tells you where to look next.
Why This Matters
Hearing loss isn’t just about missing conversations. It’s linked to social isolation, depression, and even cognitive decline. Studies show people with untreated hearing loss are twice as likely to develop dementia.
But here’s the good news: hearing aids, cochlear implants, and assistive devices work. When people get the right help, their quality of life improves dramatically. They reconnect with family, enjoy music again, and feel less frustrated.
Audiometry testing is the first step. It’s not scary. It’s not painful. It’s just the clearest way to understand your hearing-and take control of it.
Is audiometry testing painful?
No, audiometry testing is not painful. You’ll hear tones and words through headphones or a bone oscillator, and you’ll signal when you hear them. The bone oscillator may feel unusual or slightly uncomfortable, especially if you wear glasses, but it doesn’t cause pain. The test is designed to be non-invasive and safe for all ages.
How long does an audiometry test take?
A full diagnostic audiometry test typically takes 30 to 45 minutes. This includes air and bone conduction testing, speech recognition tests, and tympanometry. Screening tests, like those done in schools or workplaces, can be as short as 5 to 10 minutes but don’t provide the same level of detail.
Can I do audiometry testing at home?
Some tele-audiology platforms offer remote hearing screenings, but they’re not a replacement for a clinical test. Home apps and phone-based tests lack the calibrated equipment and controlled environment needed for accurate results. For diagnosis, treatment planning, or hearing aid fitting, a professional test in a soundproof booth is required.
What does a 40 dB hearing loss mean?
A 40 dB hearing loss at speech frequencies (500-2000 Hz) means you have mild to moderate hearing loss. You’ll likely miss soft speech, struggle in noisy environments, and have trouble hearing consonants like ‘s’, ‘f’, or ‘th’. Hearing aids are often recommended at this level to improve clarity and communication.
Do I need a referral to get an audiometry test?
No, you don’t need a referral. Audiologists are primary care providers for hearing health. You can book a diagnostic audiometry test directly with an audiology clinic, hospital audiology department, or private practice. Some insurance plans may require a referral for coverage, but it’s not medically necessary to see a doctor first.
How often should I get my hearing tested?
If you’re over 50 or regularly exposed to loud noise, get tested every year. If you’re under 50 with no risk factors, every 3 to 5 years is fine. If you notice changes-like needing the TV louder, struggling in groups, or ringing in your ears-don’t wait. Get tested right away.
Next Steps If You’re Concerned About Your Hearing
If you’ve noticed changes in your hearing, don’t wait. Start by scheduling a diagnostic audiometry test. Bring a family member if you can-they’ll hear the results too and help you remember what was said.
Write down your concerns: “I miss words in conversations,” “I can’t hear the doorbell,” “My grandchildren say I don’t listen.” These details help your audiologist understand your life, not just your audiogram.
Don’t settle for a one-size-fits-all hearing aid. Ask about advanced features like directional microphones, noise reduction, and Bluetooth streaming. Your hearing is unique. Your solution should be too.
And remember: hearing loss is not a weakness. It’s a common condition-and one that modern science can help you manage well. The first step? Know your numbers. Get tested.

Comments (12)
David vaughan
21 Nov, 2025I never realized how much detail goes into this... Seriously, the way they break down dB levels is eye-opening. I thought hearing loss was just 'everything sounds muffled'-but no, it's like your brain loses the tiny consonant bits first. That's why I keep asking people to repeat 's' and 't' words. Not being lazy. Just biology. 😅
Corra Hathaway
21 Nov, 2025Okay but can we talk about how people think hearing aids are magic glasses?? They’re not. If your brain can’t process sound, no amount of amplification fixes that. Speech discrimination testing is the REAL hero here. 🙌
jim cerqua
22 Nov, 2025This post is basically a 2,000-word ad for audiologists. Where’s the data on how many people get misdiagnosed because their audiogram didn’t match their real-life struggles? I’ve seen people with 'normal' results still crying in restaurants because they can’t follow conversations. This test doesn’t capture the chaos.
Paula Jane Butterfield
23 Nov, 2025As someone who works with deaf and hard-of-hearing communities, I’m so glad this explains bone conduction so clearly. But I wish it mentioned cochlear implants earlier-especially for parents reading this. Early intervention isn’t just 'good,' it’s life-changing. And yes, the test is non-invasive, but the fear? That’s real. Don’t underestimate that.
Simone Wood
25 Nov, 2025The Hughson-Westlake method? Really? That’s from the 40s. We’ve got AI-driven auditory profiling now in Europe. Why are we still clinging to this analog relic? The audiogram is a 2D snapshot of a 3D problem. It’s outdated. And don’t get me started on how US clinics ignore binaural integration metrics.
Clifford Temple
26 Nov, 2025I work for the VA. We test 200 vets a month. 80% of them have noise-induced loss from gunfire. They come in thinking it's 'just aging.' Nope. It's preventable. And yet, the military still doesn't mandate proper ear protection on ranges. This isn't medical-it's negligence.
Eliza Oakes
28 Nov, 2025So let me get this straight-you're telling me if I can hear a dog bark but not my kid say 'cat,' it's not me being old, it's my inner ear? And hearing aids won't fix it if my brain's broken? So what, I'm just doomed? 😭
Steve Harris
30 Nov, 2025I’ve been an audiologist for 22 years. This post nails it. But I’ll add one thing: people think the test is about hearing 'better.' It’s not. It’s about understanding 'why' you’re struggling. That’s the difference between a screening and a diagnosis. And yes, the bone oscillator feels weird. I’ve had patients cry because it tickled. It’s not pain-it’s surprise. You’re not broken. You’re just human.
Shawn Sakura
30 Nov, 2025I got tested last year after my wife said I was yelling at the TV. 38 dB loss in the high frequencies. Got hearing aids. Now I hear my grandkids say 'I love you' without asking them to repeat it. Best $2,000 I ever spent. Don’t wait till you’re missing birthdays. Just go. 🙏
Swati Jain
1 Dec, 2025In India, most people think hearing loss = old people. But my cousin, 28, works in a call center and has 45 dB loss from headset noise. No one takes it seriously. We need public campaigns. Not just clinics. This isn’t a luxury-it’s a right. And yes, I’m a jargon queen. But this stuff matters.
Florian Moser
3 Dec, 2025The most important line in this entire post: 'Hearing loss isn’t a weakness. It’s a common condition.' That’s the message we need to spread. Not shame. Not denial. Not 'just turn up the volume.' Recognition. Action. Compassion. Thank you for writing this with such clarity.
Michael Marrale
4 Dec, 2025I’ve been researching this for months. You know what they don’t tell you? The government pays audiologists to push hearing aids. The test is rigged. They want you to think you need them. But I’ve got a friend who got implants and still can’t understand his wife. The whole system is a scam. The real solution? Stop listening to noise. And maybe stop using headphones.