When your lungs start to scar, your heart doesn’t just watch-it struggles. Idiopathic pulmonary fibrosis (IPF) isn’t just a lung disease. It’s a silent force that rewires how your heart works, often pushing it to the brink. Many people think of IPF as a problem of breathing, but the real danger often lies in what happens to the heart as the disease progresses.
What Is Idiopathic Pulmonary Fibrosis?
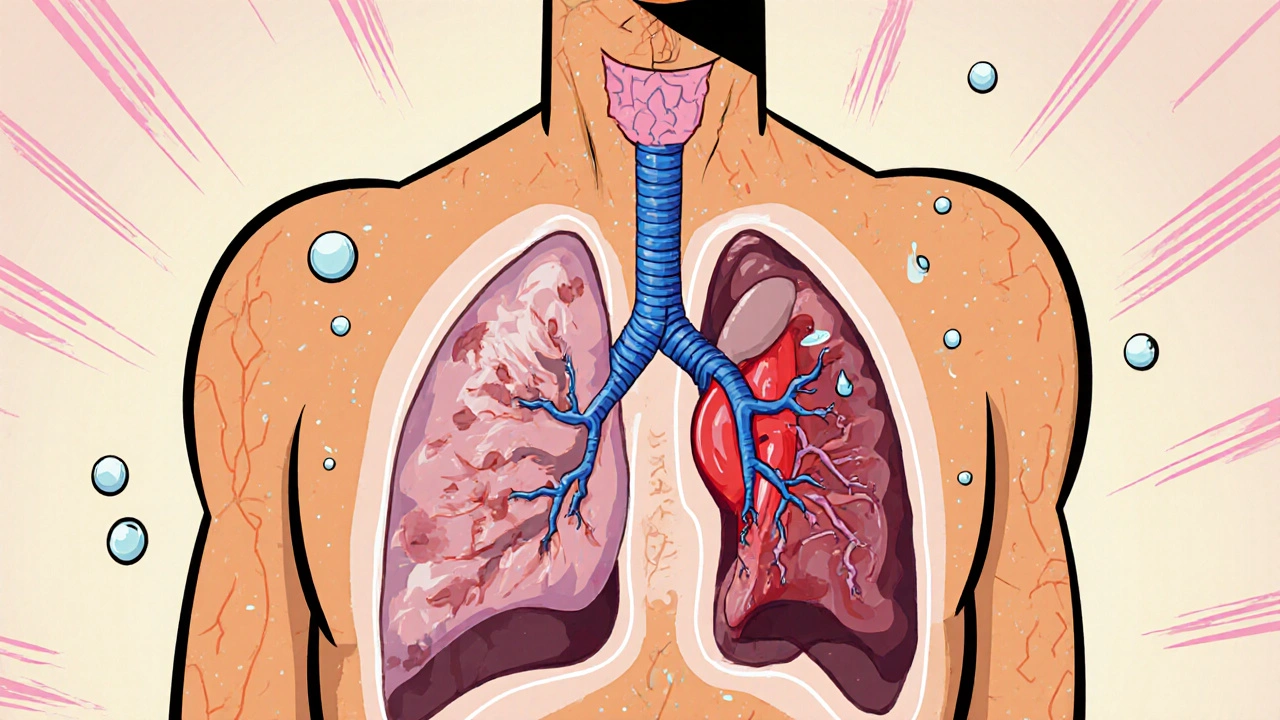
Idiopathic pulmonary fibrosis is a progressive lung disease where healthy lung tissue turns into stiff, scarred tissue over time. The cause? Unknown-hence the word “idiopathic.” This scarring, called fibrosis, makes it harder for oxygen to pass from your lungs into your bloodstream. People with IPF often feel out of breath even during simple tasks like walking to the kitchen or getting dressed.
IPF mostly affects people over 60, and it’s more common in men and former smokers. About 13 to 20 out of every 100,000 people in the U.S. have it. The average life expectancy after diagnosis is 3 to 5 years, though some live longer with careful management. There’s no cure. Treatments like pirfenidone and nintedanib can slow scarring, but they don’t reverse it.
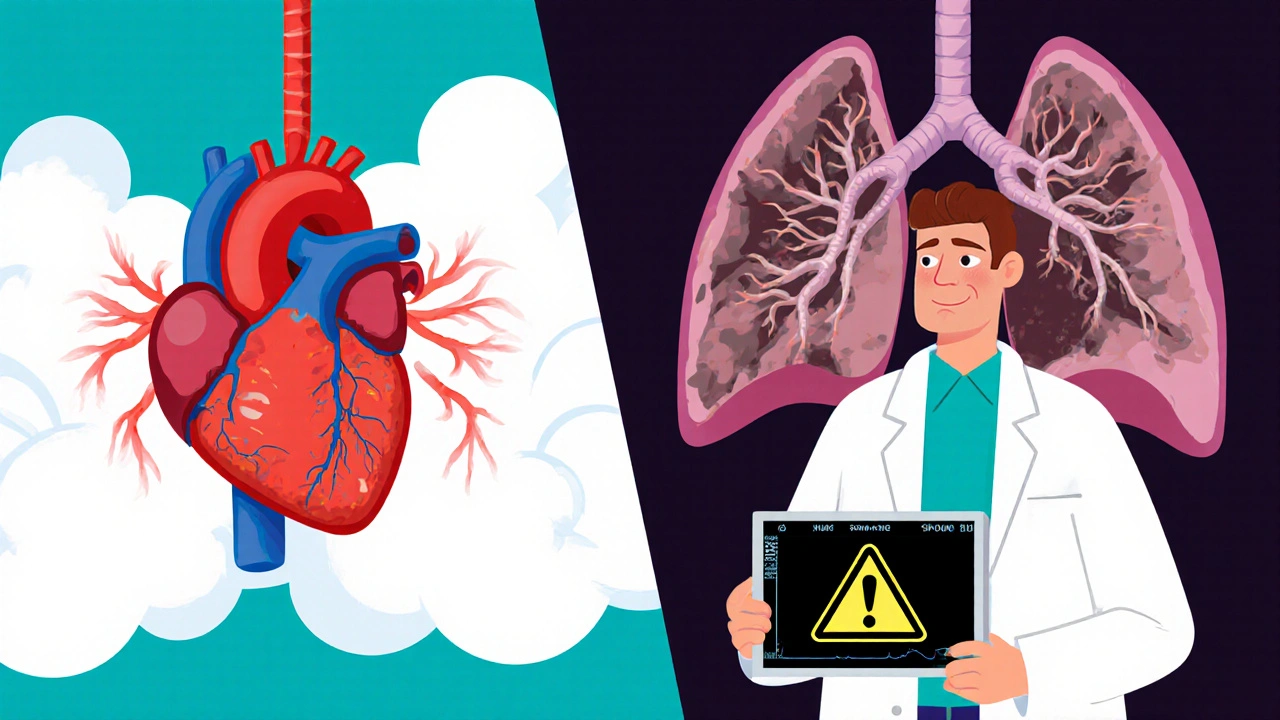
The Heart’s Response to Scarred Lungs
Your heart doesn’t just pump blood-it pumps it through your lungs to pick up oxygen. When the lungs stiffen due to IPF, the blood vessels inside them narrow and thicken. This raises pressure in the pulmonary arteries, a condition called pulmonary hypertension. It’s not the same as high blood pressure in your arms-it’s high pressure in the arteries that go from your heart to your lungs.
As that pressure climbs, the right side of your heart has to work harder. Think of it like trying to blow air through a straw that’s been pinched shut. Eventually, the muscle in the right ventricle thickens and weakens. This is called cor pulmonale-heart failure caused by lung disease. In IPF patients, up to 80% develop some degree of pulmonary hypertension by the later stages.
Heart Failure in IPF: A Common and Deadly Combo
Heart failure isn’t rare in IPF-it’s expected. Studies show that nearly half of people with advanced IPF also have signs of heart failure. And it’s not just the right side. Over time, the strain on the right heart can affect the left side too. When the left ventricle doesn’t fill properly because the right side is swollen and weak, overall blood flow drops. This leads to fatigue, swelling in the legs, and fluid buildup in the abdomen.
One 2023 study tracking 412 IPF patients found that those with pulmonary hypertension had a 3.5 times higher risk of death within a year than those without. The worse the lung scarring, the worse the heart strain. And when both organs fail together, survival drops sharply.
Why Standard Heart Treatments Don’t Always Work
Doctors often reach for diuretics, beta-blockers, or ACE inhibitors for heart failure. But in IPF, these drugs can backfire. Diuretics might help with swelling, but they can lower blood pressure too much, reducing oxygen delivery to already struggling tissues. Beta-blockers slow the heart rate, but in someone with low oxygen levels, that can make breathing even harder.
There’s no one-size-fits-all heart treatment for IPF. What works for a person with coronary artery disease might harm someone with lung scarring. That’s why managing IPF-related heart issues requires a tailored approach-often involving oxygen therapy, pulmonary rehab, and careful monitoring of blood pressure and oxygen saturation.
Signs the Heart Is Struggling
It’s easy to confuse heart problems with worsening IPF. Both cause shortness of breath and fatigue. But there are clues that point to heart involvement:
- Swelling in the ankles, legs, or belly that gets worse by evening
- Neck veins that bulge when sitting up
- Fast or irregular heartbeat, especially when resting
- Need to sleep propped up with pillows to breathe
- Sudden weight gain of 2+ pounds in a day
If you notice any of these, talk to your doctor. A simple echocardiogram can check for pulmonary hypertension and right heart strain. Blood tests like BNP can show if your heart is under stress. These aren’t routine in early IPF-but they should be if symptoms change.
Living With Both Diseases
Managing IPF and heart strain isn’t about fixing one or the other. It’s about balancing both. Oxygen therapy is often the most important tool-it reduces the pressure in lung arteries, easing the heart’s workload. Pulmonary rehab programs that include gentle exercise and breathing techniques help maintain muscle strength and reduce fatigue.
Medications like nintedanib and pirfenidone may slow lung decline, which indirectly helps the heart. But avoiding infections-like flu or pneumonia-is critical. A single respiratory infection can send both lungs and heart into crisis.
Many patients benefit from a low-sodium diet to reduce fluid retention. Limiting fluids isn’t usually needed unless swelling is severe. Staying active within your limits helps keep circulation moving and prevents blood clots.
When to Consider Advanced Care
For some, lung transplantation becomes the only option. It’s not a cure, but it can reset the heart’s burden. After transplant, pulmonary hypertension often improves dramatically, and heart function can return to near-normal. But transplant isn’t for everyone-age, other health conditions, and overall strength matter.
For those not eligible, palliative care focused on comfort and quality of life becomes essential. This includes managing symptoms, reducing anxiety, and planning ahead. The goal isn’t to extend life at all costs-it’s to make the time you have as clear and comfortable as possible.
What Research Is Showing Now
New studies are looking at how IPF and heart disease interact at the cellular level. Researchers are finding shared pathways-like chronic inflammation and oxidative stress-that damage both lung and heart tissue. Drugs targeting these pathways are in early trials. One promising area is antifibrotic agents that may protect the heart as well as the lungs.
There’s also growing interest in using wearable tech to monitor heart and lung function together. Devices that track oxygen levels, heart rate, and activity patterns can alert doctors to early signs of decline before symptoms become severe.
Final Thoughts
Idiopathic pulmonary fibrosis doesn’t just steal your breath-it strains your heart. The two are deeply connected, and ignoring one means missing the bigger picture. If you or someone you care for has IPF, pay attention to heart symptoms. Don’t assume every breathless moment is just the lungs. Ask for an echocardiogram. Monitor for swelling. Track your weight. These small steps can catch heart problems early, when they’re still manageable.
The link between lung scarring and heart failure isn’t theoretical. It’s real, common, and deadly. But with awareness, careful monitoring, and the right support, you can live better for longer.
Can idiopathic pulmonary fibrosis cause heart failure?
Yes. IPF causes scarring in the lungs, which increases pressure in the pulmonary arteries. This forces the right side of the heart to work harder, leading to right-sided heart failure, known as cor pulmonale. Studies show up to 80% of advanced IPF patients develop pulmonary hypertension, and nearly half show signs of heart failure.
Is pulmonary hypertension common in IPF patients?
Very common. Pulmonary hypertension develops in 50-80% of people with advanced IPF. It’s not just a side effect-it’s a major driver of poor outcomes. The higher the pressure in the lung arteries, the shorter the life expectancy. Regular echocardiograms are key to catching it early.
Can heart medications help IPF patients with heart strain?
Some can, but many standard heart drugs are risky. Diuretics may help with swelling but can lower blood pressure too much. Beta-blockers can slow the heart too much in low-oxygen conditions. Treatment must be personalized. Oxygen therapy and pulmonary rehab are often safer and more effective than pills.
What are the signs that IPF is affecting the heart?
Watch for swelling in the legs or belly, bulging neck veins, waking up gasping for air, rapid heartbeat at rest, or sudden weight gain. These aren’t just signs of worsening lung disease-they signal heart strain. An echocardiogram can confirm pulmonary hypertension or right heart failure.
Does lung transplant help the heart in IPF patients?
Yes. After a lung transplant, pulmonary hypertension often improves dramatically because the stiff, scarred lungs are replaced. Right heart function typically recovers over months. Many patients see their heart failure symptoms disappear. Transplant is the only treatment that can truly reset the heart-lung connection in advanced IPF.

Comments (11)
Jasmine Hwang
20 Nov, 2025bro i read this and immediately cried into my doritos
Josh Gonzales
21 Nov, 2025IPF doesn't just cause pulmonary hypertension it reshapes the entire right heart architecture over time. The right ventricle hypertrophies then dilates then fails. It's not just pressure overload it's structural remodeling. Most docs miss this because they're trained on left heart failure. Echocardiogram is non-negotiable. If you're not getting one every 6 months in advanced IPF you're not getting proper care.
Valérie Siébert
22 Nov, 2025ok but like why is everyone so obsessed with diuretics?? i had my aunt on lasix for 3 months and she was dehydrated as hell and her o2 sats dropped even more. oxygen therapy is the real MVP here. also stop making people drink water like its a wellness trend. sometimes less fluid = less struggle.
Akintokun David Akinyemi
24 Nov, 2025as a respiratory therapist in Lagos i see this daily. the heart-lung connection in IPF is brutal. patients come in gasping thinking its just their lungs but their jugulars are distended their ankles are pitting their BNP is through the roof. we push for echo early. no waiting. if you wait for classic heart failure signs its already too late. the fibrosis is stealing oxygen from the myocardium too. its a double hit. and yes nintedanib helps the heart indirectly. less fibrosis = less pressure = less strain. its not magic but its the best we got.
Adesokan Ayodeji
24 Nov, 2025hey if you or someone you love has ipf dont give up. i know its heavy but small things matter. walking around the house daily keeping salt low doing breathing exercises even if its just 5 minutes. oxygen isn't a crutch its a lifeline. and trust me your heart will thank you. i've seen people live 7+ years with good management. its not a death sentence its a marathon with pit stops. keep moving keep breathing keep asking for help. you got this.
Kaylee Crosby
26 Nov, 2025just had my dad's echo done last week and his pulmonary pressure was 58. we started him on home oxygen 2L and his walking distance doubled in 3 weeks. no meds no surgery just oxygen. i wish someone told me this sooner. if you're tired and breathless and your doctor says 'its just the IPF' push back. ask for the echo. it changes everything.
Karen Ryan
27 Nov, 2025❤️ this is the most accurate post i've seen on ipf. thank you. my mom has it and we've been fighting for proper cardiac screening for months. finally got the echo. right heart strain confirmed. now we're in pulmonary rehab. 🙏
Jack Riley
29 Nov, 2025you know what's really ironic? we treat the lungs like they're the problem but the heart is the one dying first. the fibrosis is just the slow poison. the heart is the canary. we fix the lungs we fix the heart. but we don't fix the lungs we just let the heart drown. its not a disease of the lungs its a disease of the system. we're just bad at seeing the whole machine. we fix the spark plug and ignore the fuel line. and then wonder why the car won't start
Caroline Marchetta
1 Dec, 2025oh great so now i'm supposed to believe that my 78-year-old mother's swollen ankles are 'heart strain' and not just 'old age' or 'being lazy' or 'eating too much salt'? because clearly the medical community has been lying to us for decades. 🙄 i mean sure let's throw another echo at her and another pill and another appointment while we're at it. maybe if we just stare at her EKG long enough the fibrosis will disappear. *sips wine*
katia dagenais
1 Dec, 2025you know what's missing from this entire conversation? the emotional toll. the way your partner stares at you when you can't climb the stairs. the silence when you say you're tired and they know you mean 'i can't breathe'. the guilt when you realize your oxygen tank is louder than your grandchildren's laughter. this isn't just physiology. it's grief. it's watching someone you love slowly turn into a ghost. and the worst part? you're still here. breathing. watching. waiting. for the next decline. and no drug can fix that.
Jacqueline Aslet
2 Dec, 2025It is, however, imperative to note that the conflation of pulmonary hypertension with systemic hypertension, as frequently observed in lay discourse, represents a significant conceptual misalignment that may impede optimal therapeutic decision-making. Furthermore, the assertion that diuretics are universally contraindicated in this cohort is not supported by the entirety of the current clinical literature; indeed, judicious use in the context of volume overload remains a cornerstone of palliative management. A nuanced, multidisciplinary approach is not merely advisable-it is ethically obligatory.