When your child is sick and the doctor prescribes liquid antibiotics, you breathe a sigh of relief. It’s easier to give than pills, right? But then you notice the label: discard after 10 days. You finish the course in 7 days. What do you do with the rest? Throw it out? Save it? You’re not alone. Millions of parents and caregivers face this same dilemma every year. And here’s the uncomfortable truth: liquid antibiotics don’t last. Not like pills. Not like creams. Not even like other liquids. Once you mix that powder with water, the clock starts ticking - and it ticks fast.
Why Do Liquid Antibiotics Expire So Quickly?
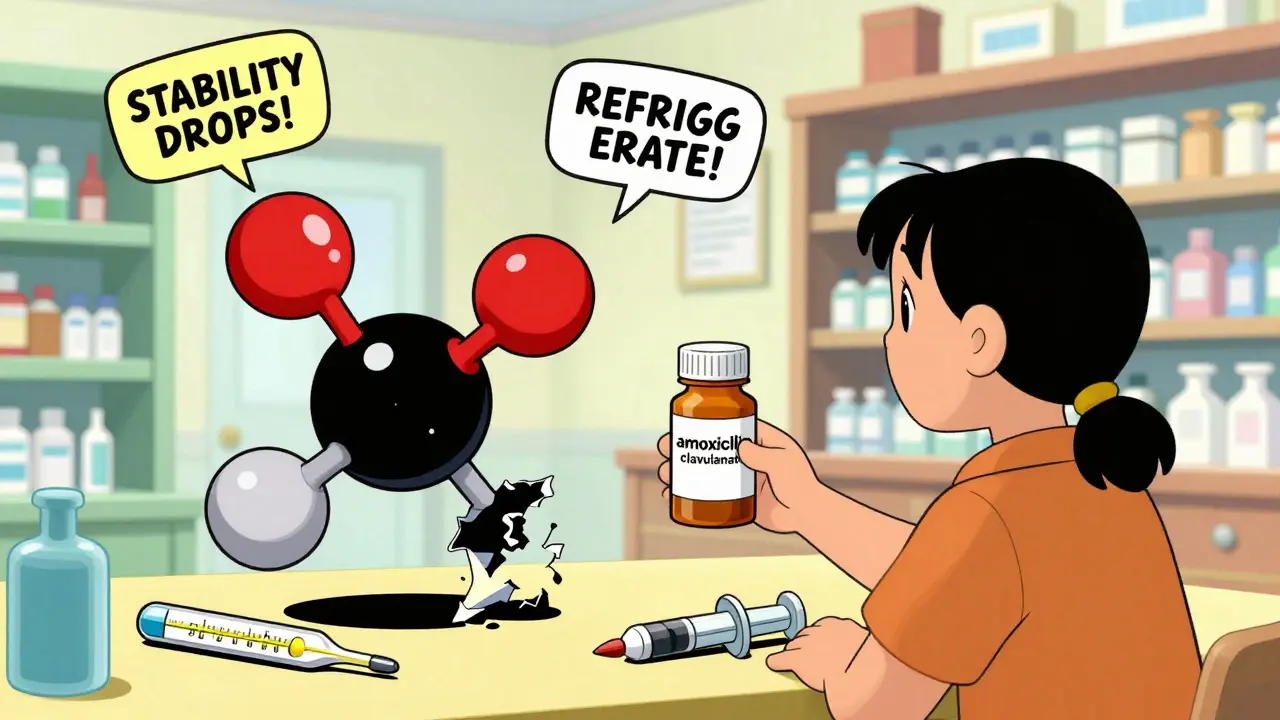
It’s not about going bad like milk. It’s about chemistry. Antibiotics like amoxicillin and ampicillin are beta-lactam compounds. In their dry powder form, they’re stable. But add water, and they start breaking down. The water molecules attack the core structure of the drug. This process is called hydrolysis. The result? Less active medicine. You might think, “But it still looks the same.” That’s the problem. You can’t tell by sight. A cloudy suspension? Maybe. A weird smell? Possibly. But often, the medicine is already losing potency - and you won’t know until it doesn’t work.
Studies show that most reconstituted suspensions must maintain at least 90% of their labeled potency to be considered effective. Once they drop below that, they’re no longer reliable. For amoxicillin alone, refrigerated (between 2°C and 8°C), that 90% threshold lasts about 14 days. But add clavulanate - the combo drug amoxicillin/clavulanate - and the clock drops to 10 days. Why? Clavulanate is even more unstable. It degrades faster. In fact, when stored in an oral syringe instead of the original bottle, clavulanate’s stability can fall below 5 days, even in the fridge. Container matters. Temperature matters. And time? It matters the most.
Storage Rules You Can’t Ignore
Refrigeration isn’t a suggestion. It’s a requirement. Keep your liquid antibiotics between 2°C and 8°C. That’s your fridge’s main compartment - not the door. Door shelves fluctuate in temperature every time you open them. Even a few hours at room temperature (above 25°C) can cut your shelf life in half. One study found that amoxicillin/clavulanate stored at 27-29°C lasted only five days before dropping below 90% potency. That’s not a typo. Five days. Not ten. Not fourteen.
Don’t transfer the medicine to another container. That includes oral syringes, even if they’re clean. The original bottle is designed with materials that protect the drug. Syringes? They can leach chemicals or allow air in. Tu et al. (1988) showed clavulanate stability dropped from 11.1 days in the original container to under 5 days in a syringe - even when kept cold. And don’t freeze it unless you’re planning to use it later. While freezing can extend shelf life to 60 days (as shown in Allen and Lo, 1979), thawing and refreezing can cause uneven degradation. Plus, once thawed, you still have to follow the 10- or 14-day rule.
What Happens If You Use Expired Liquid Antibiotics?
Let’s be clear: taking expired liquid antibiotics won’t poison you. But it might not help you either. You could end up with a lingering infection because the medicine no longer has enough strength to kill the bacteria. That’s not just inconvenient - it’s dangerous. Underdosed antibiotics are one of the main drivers of antibiotic resistance. Bacteria that survive treatment adapt. They learn. And next time, they’re harder to kill.
Pharmacists report that 22% of patients accidentally use expired reconstituted suspensions. Why? They forget the date. They think, “It’s only a few days past.” Or worse - they’re told to take the medicine for 14 days, but the bottle says “discard after 10.” That mismatch is real. One parent on Drugs.com shared that their child’s infection returned because they had to throw out the medicine on day 10, even though the prescription called for two weeks. The system doesn’t always line up.
Amoxicillin vs. Amoxicillin/Clavulanate: A Clear Difference
Not all liquid antibiotics are the same. Amoxicillin alone? It’s the more stable one. Refrigerated, it holds up for up to 14 days. Amoxicillin/clavulanate? That combo? 10 days max. Why? Clavulanate is added to fight resistant bacteria, but it’s chemically fragile. It breaks down faster than amoxicillin. Even in the same bottle, the clavulanate component degrades first. That’s why manufacturers set the discard date based on the least stable ingredient.
And it gets worse. If you’re using an oral syringe to give the medicine, the clavulanate degrades even faster. A 2022 study found that after just 3 days in a syringe, clavulanate levels dropped by 15%. That’s not just a little loss - it’s enough to reduce effectiveness. So if you’re giving a combination drug, stick to the original bottle. Use a syringe only to draw the dose, then return the rest to the bottle immediately. Don’t leave it sitting in the syringe overnight.
What Do Experts Say?
Dr. Iroanya, cited by SingleCare, says plainly: “Amoxicillin is stable for 14 days in a refrigerator after being reconstituted.” But Dr. Genovese adds a warning: “Liquid amoxicillin can degrade and become unusable even when stored in the refrigerator” if kept too long. There’s no gray area here. The 14-day window is the maximum. Not the goal. Not the average. The maximum.
Pharmaceutical guidelines from the USP and FDA aren’t arbitrary. They’re based on real data. The 14-day standard for amoxicillin and 10-day for the combo weren’t chosen because they’re convenient. They were chosen because that’s when the drug drops below 90% potency. And that 90% isn’t a random number - it’s the threshold regulators use to ensure the medicine still works. Anything less? You’re gambling.

Real Problems, Real Solutions
Here’s what actually happens in homes: parents forget the date. Kids don’t finish the course. The bottle sits on the counter. The fridge door gets opened too often. The medicine gets left out during a trip. All of it shortens the clock.
So what can you do?
- Write the discard date on the bottle the moment the pharmacist hands it to you. Don’t trust your memory.
- Store it in the back of the fridge, where it’s coldest and most stable.
- Never transfer to syringes for storage. Use the syringe only to draw the dose.
- Check for changes. If it smells bad, looks cloudy, or has particles - toss it. Even if it’s before the date.
- Use reminders. Apps like CVS’s Script Sync send alerts when the discard date is near. That’s not fluff - it cuts misuse by 18%.
And if you’re prescribed a 14-day course but the bottle says “discard after 10”? Ask your pharmacist. They might be able to dispense a second bottle with a later reconstitution date. Or they might suggest switching to a solid form if your child can swallow it.
The Bigger Picture
Reconstituted antibiotics make up about 15% of all antibiotic prescriptions in the U.S. - and 85% of those are for kids. That’s a lot of bottles being opened, used, and thrown away. The industry keeps these short shelf lives because it’s cheaper than doing long-term stability testing. It’s also safer - if you set the discard date too high, you risk people taking ineffective medicine. So manufacturers play it conservative.
But change is coming. New formulations are being tested. One 2021 study used microencapsulation to extend amoxicillin/clavulanate stability to 21 days. Pfizer’s “AmoxiClick” system, launching in 2024, separates the powder and liquid until use - potentially giving you 30 days of stability. These are promising. But they’re not here yet. For now, the rules haven’t changed.
And that’s the reality: liquid antibiotics are a tool. A helpful one. But they’re not permanent. Their short life isn’t a flaw - it’s a feature of their chemistry. The best thing you can do is respect the clock. Write the date. Keep it cold. Don’t guess. And if you’re unsure? Call your pharmacist. Better safe than sorry - especially when it comes to your child’s health.
Can I freeze liquid antibiotics to make them last longer?
Freezing can extend the shelf life of some liquid antibiotics - studies show amoxicillin and ampicillin can retain potency for up to 60 days at -20°C. But once thawed, you still must follow the original discard date (usually 10 or 14 days). Repeated freezing and thawing can damage the formulation. Unless your pharmacist specifically advises freezing, it’s not recommended for everyday use.
What if I left my child’s antibiotic on the counter overnight?
If it was left at room temperature (above 25°C) for more than a few hours, especially beyond the first day after reconstitution, the medicine may have lost potency. For amoxicillin/clavulanate, even a single night on the counter can reduce effectiveness. When in doubt, throw it out. It’s not worth the risk of incomplete treatment.
Why does the discard date differ from the prescription length?
The discard date is based on how long the medicine stays potent after mixing. The prescription length is based on how long you need to treat the infection. They don’t always match. For example, you might be prescribed a 14-day course, but the liquid antibiotic must be discarded after 10 days. Talk to your pharmacist - they can often provide a second bottle or switch to a solid form to avoid waste.
Is it safe to use liquid antibiotics past the discard date if they look fine?
No. Even if the liquid looks clear and smells normal, its potency may have dropped below the 90% threshold required to be effective. You can’t see, smell, or taste degradation. Using expired antibiotics increases the risk of treatment failure and antibiotic resistance. Always follow the discard date.
Can I save leftover liquid antibiotics for next time?
No. Liquid antibiotics are meant for one specific infection, at one specific time. Bacteria change. Dosages change. Your child’s weight changes. Even if the medicine looks good, it’s not safe to reuse. Storing it for future use increases the risk of giving an incorrect dose or using an ineffective drug. Always get a fresh prescription for a new illness.
Next time you’re handed a bottle of liquid antibiotic, don’t just take it. Ask: When was it mixed? Where should it go? When does it expire? A few seconds of attention now can prevent a longer, harder illness later.


Comments (11)
James Lloyd
16 Feb, 2026Let’s cut through the noise: the 10- to 14-day shelf life isn’t arbitrary-it’s rooted in hydrolytic degradation kinetics of beta-lactam rings. Amoxicillin’s lactam bond cleaves in aqueous environments, and even at 4°C, the rate constant is non-trivial. The FDA’s 90% potency threshold isn’t a suggestion; it’s the lower bound of therapeutic efficacy. Anything below that is pharmacologically inert, not ‘just a little weaker.’ You’re not saving money by keeping it-you’re risking treatment failure and fostering resistance. The data doesn’t lie: storage in syringes accelerates degradation due to increased surface area and potential leaching. Stick to the bottle. Keep it cold. Trust the label. It’s science, not superstition.
Logan Hawker
17 Feb, 2026Oh, I’m so glad we’re finally talking about this-because, honestly, who hasn’t stared at a half-used bottle of amoxicillin-clavulanate like it’s a cryptic hieroglyph? I mean, I’ve got a 14-day script, but the bottle says ‘discard after 10’? That’s not a medical instruction-that’s a passive-aggressive note from Big Pharma. And don’t even get me started on the fridge door! I’ve seen moms treating antibiotics like a six-pack of soda. It’s not a snack. It’s a precision chemical. Also, why do we still use glass bottles that shatter like a breakup text? I’d pay triple for a child-safe, shockproof, temperature-stable, app-synced vial. And yes-I’ve Googled ‘amoxicillin drone delivery.’ I’m not alone.
Digital Raju Yadav
19 Feb, 2026This is why India produces 20% of the world’s generic antibiotics and you still have to throw half away. Weak science. Weak regulation. Weak culture of responsibility. In my country, we don’t have ‘discard dates’-we have ‘use before it stops working’-and that’s based on experience, not some American lab report. You think refrigeration fixes everything? In Mumbai, the power cuts last 8 hours. What do you do then? Cry? No. You give the medicine. And if the child gets better? Good. If not? You try again. This over-analyzing is a luxury of rich nations. We don’t have the luxury of discarding 40% of our meds. You call it ‘safety.’ We call it waste.
Carrie Schluckbier
19 Feb, 2026Wait-so you’re telling me the government and pharmaceutical companies are deliberately keeping shelf life short so we keep buying more? And they’re using ‘stability studies’ as a cover? I’ve read the patents. The microencapsulation tech has existed since 2018. Pfizer’s AmoxiClick? It’s not ‘coming soon’-it’s already in trials. Why isn’t it everywhere? Because if you could store liquid antibiotics for 30 days, parents wouldn’t need to refill. And if they didn’t refill? Pharma loses billions. This isn’t chemistry-it’s corporate calculus. They want you scared. They want you confused. They want you buying new bottles. I’ve got screenshots. I’ve got internal memos. This is a scam. And you’re all just swallowing it-literally.
Liam Earney
21 Feb, 2026You know, I find it deeply unsettling how casually we treat these substances-like they’re just… syrup. As if the molecular integrity of a beta-lactam antibiotic is something we can negotiate with, like a parking ticket. I mean, I’ve held bottles in my hands, and I’ve felt the weight of that fragility-not just chemical, but existential. The fact that a child’s life hinges on whether a bottle was stored three inches deeper in the fridge… it’s absurd. It’s tragic. It’s a microcosm of how we’ve outsourced care to systems that don’t care. And yet, we blame the parent for forgetting the date. We blame the child for not finishing. We blame the pharmacist for not being clearer. But who designed the system? Who decided that 10 days was acceptable? And why do we accept it without screaming?
guy greenfeld
22 Feb, 2026It’s not about the antibiotic. It’s about time. We live in a world where everything is disposable, even healing. We treat medicine like a subscription-buy it, use it, toss it, buy again. But what does that say about us? That we’ve lost the patience to let the body heal? That we’ve replaced ritual with regulation? The discard date isn’t a chemical truth-it’s a cultural one. We’ve forgotten how to wait. How to trust. How to let a child rest, not just medicate. The real crisis isn’t degradation-it’s our inability to sit with uncertainty. We need a pill for everything. Even for the silence between doses.
Adam Short
23 Feb, 2026Let me tell you something about British pharmacies: we don’t have this problem. We have a national health system that doesn’t outsource stability testing to profit-driven labs. We have pharmacists who actually *talk* to parents. We have prescriptions printed with the discard date, the storage instructions, and a bloody QR code that links to a video. We don’t have parents guessing. We don’t have ‘what ifs.’ We have clarity. And yes, I know this is the US, but you know what? You’re doing it wrong. You’ve turned a medical necessity into a logistical nightmare because you’ve outsourced empathy to a corporate flowchart. Fix your system. Or stop pretending you care about children.
Sam Pearlman
24 Feb, 2026Okay, but hear me out-what if we just… didn’t use liquid antibiotics at all? Like, why are we even giving them in the first place? Kids can swallow pills now. We’ve got chewables. We’ve got flavored capsules. We’ve got patches. Why are we still mixing powders like it’s 1998? I’ve got a 5-year-old who eats antibiotics like gummy worms. No mess. No fridge. No ‘discard by’ panic. Maybe the real solution isn’t better storage-it’s better delivery systems. And if Big Pharma won’t make them? We should boycott liquid forms until they do. Seriously. Vote with your wallet. No more syrup. No more bottles. No more ‘I forgot the date.’
Steph Carr
26 Feb, 2026Oh honey, I’ve been there. I’ve had the bottle on the counter, the syringe full overnight, the ‘but it still looks fine!’ argument. And then I Googled ‘amoxicillin degradation products’ and saw the chemical structures of N-oxide and penicilloic acid. I cried. Not because I’m dramatic-because I realized I’d been treating my child’s infection with soup. Soup made from broken molecules. And then I called the pharmacist. They said, ‘Yeah, we know. We’re just waiting for the FDA to catch up.’ So I made a spreadsheet. I track every bottle. I label it with a Sharpie. I set three phone alarms. And I refuse to let another parent feel the panic I felt. If you’re reading this-you’re not alone. And you’re not failing. You’re just in a system that forgot to put a safety net under the ladder.
Brenda K. Wolfgram Moore
28 Feb, 2026Thank you for writing this. I’ve been a nurse for 18 years and I’ve seen too many kids get sicker because parents reused old antibiotics. It’s not laziness-it’s fear. Fear of cost. Fear of another doctor visit. Fear of being told they’re wrong. But the truth is, we’re not teaching people how to handle this. We’re just handing them a bottle and saying ‘do this.’ No one shows them how to store it. No one explains why. No one says, ‘If you’re unsure, call us-we’ll help.’ We need a national campaign. A simple poster. A video. A checklist. Something that says: ‘This medicine is alive. It’s breathing. It’s dying. Don’t let it die before your child heals.’
Linda Franchock
1 Mar, 2026Look-I get it. You’re tired. You’re overwhelmed. You just want your kid to feel better. But here’s the thing: you don’t have to be perfect. You just have to be consistent. Write the date on the bottle. Put it in the back of the fridge. Don’t leave it in the syringe. And if you’re confused? Call the pharmacy. They’ve got a line for this. They’ve seen it a hundred times. You’re not bothering them. You’re helping them help you. And if you accidentally leave it out? Don’t panic. Just throw it out. No guilt. No shame. Your kid’s health isn’t a test. It’s a gift. And you’re doing better than you think.