Diabetes Medication Sugar Impact Calculator
How Your Diet Affects Medication
This tool helps you understand how your sugar intake impacts the effectiveness of your diabetes medication. Based on the latest research, we'll show you how much additional medication you might need and the potential risks of high sugar intake.
Your Results
Recommended Changes
When you’re taking diabetes medication, what you eat matters just as much as the pill you swallow. Many people think that popping a metformin tablet means they can eat whatever they want - but that’s not how it works. High sugar intake doesn’t just raise your blood glucose; it can make your medication less effective, increase side effects, and even put you at risk for dangerous highs or lows. The truth is, your diabetes meds and your diet are a team. If one is weak, the whole system suffers.
How Sugar Undermines Diabetes Medications
Diabetes medications like metformin, sulfonylureas, and GLP-1 agonists don’t magically erase sugar from your bloodstream. They help your body manage it better - but they can’t keep up if you flood your system with it. For example, metformin works by slowing down how much sugar your liver releases and helping your muscles absorb glucose more efficiently. But if you drink a 20-ounce soda with 65 grams of sugar, your body gets hit with more glucose than even the strongest dose of metformin can handle. A 2022 GoodRx analysis found that people who ate over 100 grams of added sugar daily needed nearly 30% more metformin just to get the same blood sugar control as those who kept added sugar under 25 grams.
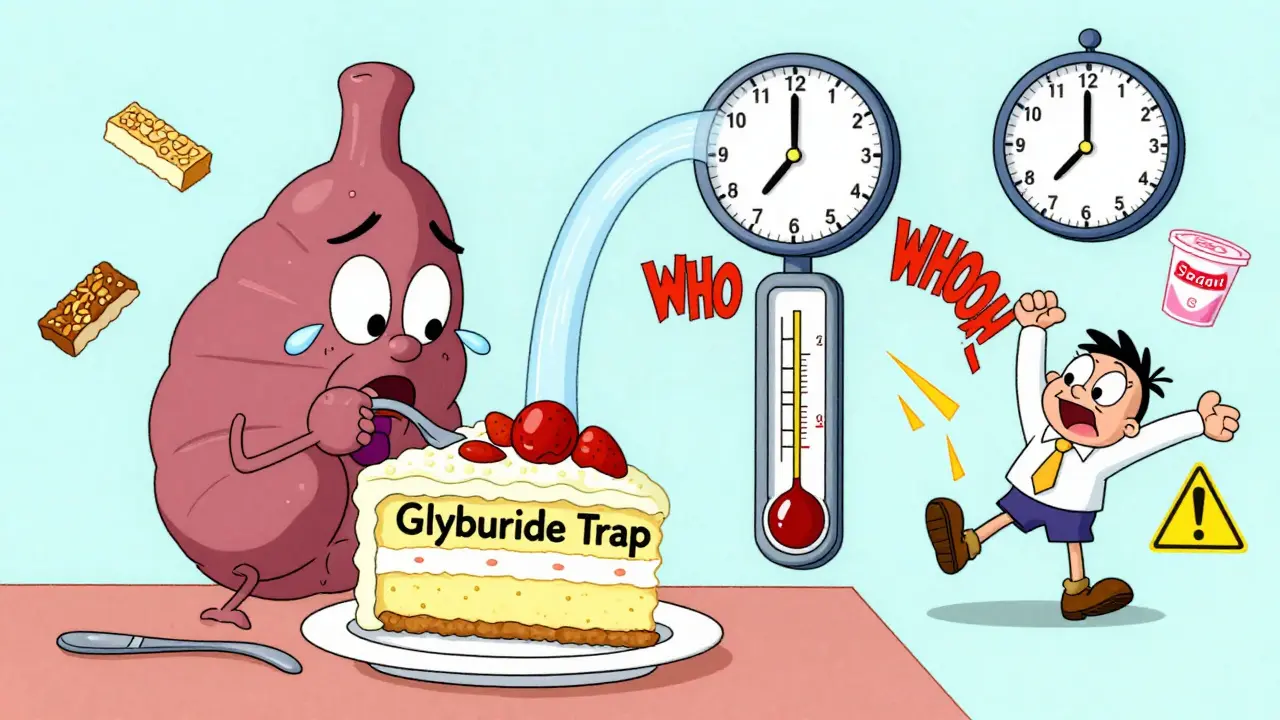
Other medications are even more sensitive. Sulfonylureas like glipizide and glyburide force your pancreas to pump out more insulin. That’s great - until you skip a meal or eat a huge sugary snack. If you eat a big slice of cake after taking your pill, your insulin spikes and your blood sugar crashes hours later. The Cleveland Clinic reports that 68% of patients on glyburide experience dangerous low blood sugar 3 to 5 hours after a high-carb meal. That’s not a coincidence - it’s a direct result of mismatched food and medicine.
What Foods to Avoid With Diabetes Medications
Not all sugar is the same, but most of the worst offenders are hidden. Here are the top seven food categories to watch out for if you’re on diabetes meds:
- Sugary drinks: Soda, sweetened iced tea, fruit juice with more than 20g sugar per serving. One can of soda can have more sugar than the entire daily limit recommended by the American Diabetes Association.
- High-sugar fruits: Mangoes, grapes, cherries, and pineapple can spike blood sugar fast - especially if eaten alone without fiber or protein.
- Processed snacks: Granola bars, cookies, packaged muffins, and even "healthy" cereals often contain over 15g of added sugar per serving. Check labels - sugar hides under 60+ names like high-fructose corn syrup, cane juice, and dextrose.
- High-fat meals: Fried foods, fatty meats, and creamy sauces slow digestion. This delays how quickly your medication kicks in, causing unpredictable blood sugar spikes hours later.
- Sweetened dairy: Flavored yogurts, pudding cups, and sweetened almond milk often contain 15g or more of sugar. Plain Greek yogurt with a handful of berries is a far better choice.
- Alcohol with mixers: Sweet cocktails, sangria, and pre-mixed drinks pack 25g or more of sugar. Even beer and wine can interfere with how your liver releases glucose, increasing hypoglycemia risk, especially with insulin or sulfonylureas.
- Refined carbs: White bread, pastries, and instant oatmeal break down into pure glucose. They spike blood sugar faster than table sugar and leave you hungry again in an hour.
The NHS warns that consuming sugary drinks while on metformin requires checking your blood sugar every two hours for six hours afterward. That’s not an exaggeration - it’s a safety step for people who’ve seen their levels shoot up to 250 mg/dL or higher after just one sugary drink.
Why Low-Glycemic Foods Work Better With Meds
Not all carbs are enemies. The key is how fast they turn into sugar in your blood. Low-glycemic-index (GI) foods - those with a GI under 55 - release glucose slowly, giving your medication time to work. A 2025 review in the International Journal of Molecular Sciences found that switching from high-GI to low-GI foods improved insulin sensitivity by 25-40% and cut post-meal glucose spikes by 35-50 mg/dL on average.
Examples of low-GI foods that pair well with diabetes meds:
- Steel-cut oats instead of instant oatmeal
- Quinoa or brown rice instead of white rice
- Legumes like lentils, chickpeas, and black beans
- Non-starchy vegetables: broccoli, spinach, zucchini, cauliflower
- Most berries: strawberries, raspberries, blueberries
- Nuts and seeds: almonds, chia, flax
These foods don’t just help your meds work better - they keep you full longer, reduce cravings, and stabilize your energy. That’s why people using continuous glucose monitors (CGMs) report 47% less time spent in high blood sugar when they swap out refined carbs for low-GI options.
Medications That Are More Forgiving - But Still Need Limits
Some newer diabetes drugs are more forgiving when it comes to sugar intake. SGLT2 inhibitors like dapagliflozin and canagliflozin work by making your kidneys flush out extra glucose through urine. That means they’re less affected by what you eat. GLP-1 agonists like semaglutide slow digestion, reduce appetite, and help your body use insulin more naturally. Studies show these drugs still work at 85-90% of their full power even with moderate sugar intake.
But here’s the catch: they’re not magic. The American Diabetes Association’s 2023 guidelines say even these newer medications lose 15-20% of their effectiveness when patients regularly consume over 100g of added sugar daily. That’s the equivalent of five cans of soda. You still need to manage sugar - just not as strictly as someone on sulfonylureas.
What Happens When You Ignore the Diet
Ignoring dietary advice doesn’t just mean your blood sugar stays high. It can lead to real health consequences:
- Higher doses needed: You might need more medication, which increases cost and side effects.
- More hypoglycemia: Especially with insulin or sulfonylureas - low blood sugar can cause dizziness, confusion, seizures, or even coma.
- Increased risk of lactic acidosis: With metformin, high sugar intake combined with poor kidney function (eGFR under 45) can raise lactic acid levels dangerously. Case reports show a 3.2-fold increase in risk.
- Slower progress: People who get diet counseling along with their meds reach target HbA1c levels in 6.2 months - nearly five months faster than those who only take pills.
And it’s not just about numbers. A 2023 study from the T1D Exchange registry showed that people who consistently tracked carbs with their insulin pumps had HbA1c levels 0.8% lower on average. That might sound small, but it means a 35% lower risk of kidney damage, nerve problems, and vision loss over time.

Why Most People Don’t Get the Right Advice
Here’s the uncomfortable truth: most doctors don’t talk about diet enough. A 2023 NIDDK survey found that only 39% of primary care providers refer newly diagnosed Type 2 patients to a registered dietitian. The American Diabetes Association says everyone starting diabetes meds should see a dietitian within 30 days. But only 42% of healthcare systems follow that rule.
That’s a gap. A big one. Patients who complete a 12-week nutrition program while starting meds need 63% fewer emergency visits for blood sugar crises and require 2.5 fewer medication adjustments in their first year. Yet, most people are handed a prescription and told to "eat healthier" - without a plan.
Don’t wait for your doctor to bring it up. Ask for a referral. Look for a registered dietitian who specializes in diabetes. They’ll help you build a real, sustainable plan - not just a list of "don’t eat this." They’ll show you how to balance meals, read labels, and match your food to your medication schedule.
Practical Tips to Start Today
You don’t need to overhaul your life overnight. Start with these five steps:
- Swap one sugary drink per day: Replace soda or sweetened coffee with sparkling water, unsweetened tea, or infused water with lemon or mint.
- Check labels before buying: If a product has more than 5g of added sugar per serving, think twice. Avoid anything listing sugar, syrup, or juice concentrate in the first three ingredients.
- Pair carbs with protein or fat: Eat an apple with a handful of almonds. Have oatmeal with chia seeds and peanut butter. This slows sugar absorption.
- Time your meals: If you’re on sulfonylureas or insulin, eat about the same amount of carbs at each meal. Don’t skip breakfast or eat a huge dinner.
- Use a CGM if you can: Even a short-term rental can show you exactly how your favorite foods affect your blood sugar. Real data beats guesswork every time.
Small changes add up. One person in Wellington reduced her HbA1c from 8.1% to 6.4% in six months just by cutting out sugary drinks and switching to whole grains. She didn’t change her meds. She just changed her plate.
Final Thought: Your Meds Can’t Do It Alone
Diabetes isn’t just a pill problem. It’s a lifestyle problem - and food is the biggest lever you have. No medication, no matter how advanced, can undo the damage of constant sugar overload. But when you pair smart eating with your meds, you’re not just controlling your blood sugar - you’re taking back control of your health.
Can I still eat fruit if I have diabetes and take metformin?
Yes, but choose wisely. Berries, apples, pears, and citrus fruits have lower sugar and high fiber, making them better choices. Avoid mangoes, grapes, and dried fruit in large amounts. Eat fruit with a source of protein or fat - like a handful of nuts - to slow sugar absorption. A serving of fruit should be about one small piece or 1/2 cup chopped.
Does alcohol affect diabetes medications differently than sugar?
Yes. Alcohol itself can lower blood sugar, especially when taken on an empty stomach or with insulin or sulfonylureas. Sweet cocktails add sugar on top of that, creating a double risk: high sugar spikes followed by dangerous lows. Stick to dry wine, light beer, or spirits with soda water and lime. Never drink alcohol without eating, and check your blood sugar before bed if you’ve had any.
Is it safe to take metformin with high-fat meals?
It’s not ideal. High-fat meals slow down how fast your stomach empties, which delays metformin absorption. This can cause unpredictable blood sugar spikes later. While metformin doesn’t interact chemically with fat, the timing of your dose matters. Take it with food to reduce stomach upset, but avoid meals heavy in fried foods, butter, or cream. Lean proteins and healthy fats (like avocado or olive oil) are better.
Why do some people need more metformin than others?
It’s often not about body weight or genetics - it’s about diet. People who eat over 100g of added sugar daily may need higher doses because their bodies are constantly flooded with glucose. Metformin can only do so much. Reducing sugar intake often allows doctors to lower the dose, reducing side effects like nausea or diarrhea. Your dose isn’t fixed - it’s a response to your lifestyle.
Can I stop my diabetes meds if I eat better?
Some people can - but only under medical supervision. Losing weight, cutting sugar, and exercising can improve insulin sensitivity enough that some individuals reduce or even stop medication. But never stop on your own. Stopping suddenly can cause dangerous blood sugar spikes. Work with your doctor and a dietitian to monitor progress safely.
How long does it take to see results from diet changes with diabetes meds?
You might notice less hunger and more stable energy within days. Blood sugar readings often improve in 1-2 weeks. HbA1c levels - which show your average blood sugar over 3 months - typically drop by 0.5% to 1.5% within 3-6 months with consistent changes. The key is consistency, not perfection.
Managing diabetes isn’t about restriction - it’s about empowerment. When you understand how your food and meds work together, you’re no longer just reacting to numbers on a screen. You’re building a life where your health is in your hands.


Comments (20)
Michael Bond
26 Dec, 2025Just swapped soda for sparkling water with lime. My BG dropped 30 points in a week. No magic, just less sugar.
carissa projo
27 Dec, 2025It’s not about willpower-it’s about understanding that your body isn’t a vending machine. You don’t feed a car diesel and expect it to hum like a Tesla. Your pancreas? Same deal. When you flood it with sugar, it doesn’t just get tired-it starts screaming. And your meds? They’re just the bandages on a wound that keeps reopening. The real healing starts when you stop asking for permission to eat better and start treating your body like the miracle it is.
josue robert figueroa salazar
28 Dec, 2025metformin and soda? bro you're just wasting your money and your pancreas
christian ebongue
29 Dec, 2025oh cool so now i need to read labels like i'm decoding nasa blueprints just to eat a granola bar? thanks for the 2025 review that probably cost 50k to write
jesse chen
30 Dec, 2025I really appreciate how detailed this is. I’ve been on metformin for five years, and honestly, I didn’t realize how much my evening snack of yogurt with honey was wrecking my numbers. Switching to plain Greek yogurt and a few blueberries? Game-changer. I’ve had way fewer lows since. Thank you for the clarity.
Joanne Smith
1 Jan, 2026Let’s be real-most of these ‘dietitian referrals’ are a joke. I asked my doc for one. Got a pamphlet titled ‘Eating Well With Diabetes’ and a coupon for a smoothie place that had 42g of sugar per serving. Thanks, healthcare system.
Alex Ragen
1 Jan, 2026It’s fascinating how society treats diabetes as a personal failure, when the real failure is a medical system that prescribes pills and then expects patients to become nutritional scientists overnight-without training, without support, without even a dictionary of sugar aliases.
Kuldipsinh Rathod
2 Jan, 2026in india, we think mangoes are healthy, but now i see why my sugar spikes after eating them. i will try with almonds now.
SHAKTI BHARDWAJ
2 Jan, 2026THIS IS ALL A LIE. I EAT DONUTS AND MY GLUCOSE IS FINE. DOCTORS ARE JUST TRYING TO SELL YOU MORE DRUGS. #DIABETESCONSPIRACY
Matthew Ingersoll
3 Jan, 2026There’s a cultural component here that rarely gets discussed. In many households, food is love. To tell someone to stop eating the sweet rice their grandmother made every Sunday isn’t just dietary advice-it’s asking them to sever a thread of identity. The real challenge isn’t the sugar-it’s the grief of letting go.
david jackson
4 Jan, 2026Let me tell you what happened last week. I had a craving for cake-like, soul-crushing, can’t-sleep-without-it kind of craving. I ate a whole slice. Then I checked my CGM. My blood sugar didn’t just spike-it did a backflip, went to 298, and stayed there for three hours. I felt like a robot with a glitched algorithm. And then I cried. Not because I was mad at myself-because I realized I’d been treating my body like a broken appliance I could just reset. It’s not broken. It’s trying to survive the mess we made. And now? I’m learning to listen.
Jody Kennedy
4 Jan, 2026Y’all need to stop acting like this is hard. It’s not. It’s just different. I used to drink 3 energy drinks a day. Now I drink 3 cups of green tea. I sleep better. I don’t crash. I don’t feel like I’m running on fumes. You don’t need to be perfect. You just need to start. One swap. One day. One choice. That’s all it takes.
Prasanthi Kontemukkala
4 Jan, 2026My cousin in Delhi was told to cut sugar and started eating more lentils and leafy greens. She didn’t change her meds. Her HbA1c dropped from 8.7 to 6.9 in 5 months. Simple. Real. Powerful. You don’t need a diet plan-you need consistency. And maybe a little bit of patience.
Lori Anne Franklin
6 Jan, 2026im so bad at this but i just switched to unsweetened almond milk and i feel less foggy?? maybe im not a lost cause??
Bryan Woods
7 Jan, 2026It is worth noting that the correlation between sugar intake and medication efficacy is well-documented in peer-reviewed literature, including studies published in Diabetes Care and The Lancet Diabetes & Endocrinology. While lifestyle modification remains foundational, pharmacological outcomes are demonstrably improved with dietary adherence.
carissa projo
7 Jan, 2026And for everyone who says, ‘But I can’t give up my favorite foods’-you don’t have to. You just have to change the rhythm. Have the cake on Sunday, not every day. Savor it slowly. Make it a ritual, not a reflex. That’s not deprivation. That’s reverence.
jesse chen
8 Jan, 2026Thank you for saying that. I started doing exactly that-saving my favorite treats for weekends, and eating them mindfully. It’s not about denying myself. It’s about honoring myself. And honestly? It tastes better that way.
Joanne Smith
9 Jan, 2026And if your doctor won’t refer you to a dietitian? Go to one anyway. I paid $80 out of pocket. Best $80 I ever spent. They taught me how to read labels, plan meals around my meds, and stop feeling guilty for eating rice. You deserve that support.
Matthew Ingersoll
10 Jan, 2026That’s the quiet revolution no one talks about. It’s not about losing weight or hitting a number. It’s about reclaiming your relationship with food-not as an enemy, not as a reward, but as nourishment. And that’s worth more than any pill.
david jackson
10 Jan, 2026I’m still learning. Some days I eat clean. Some days I eat the whole bag of cookies. But now I know why. And I’m not ashamed anymore. I’m just… aware. And awareness? That’s the first step to real change.