Medication Safety Checker
Check Medication Safety
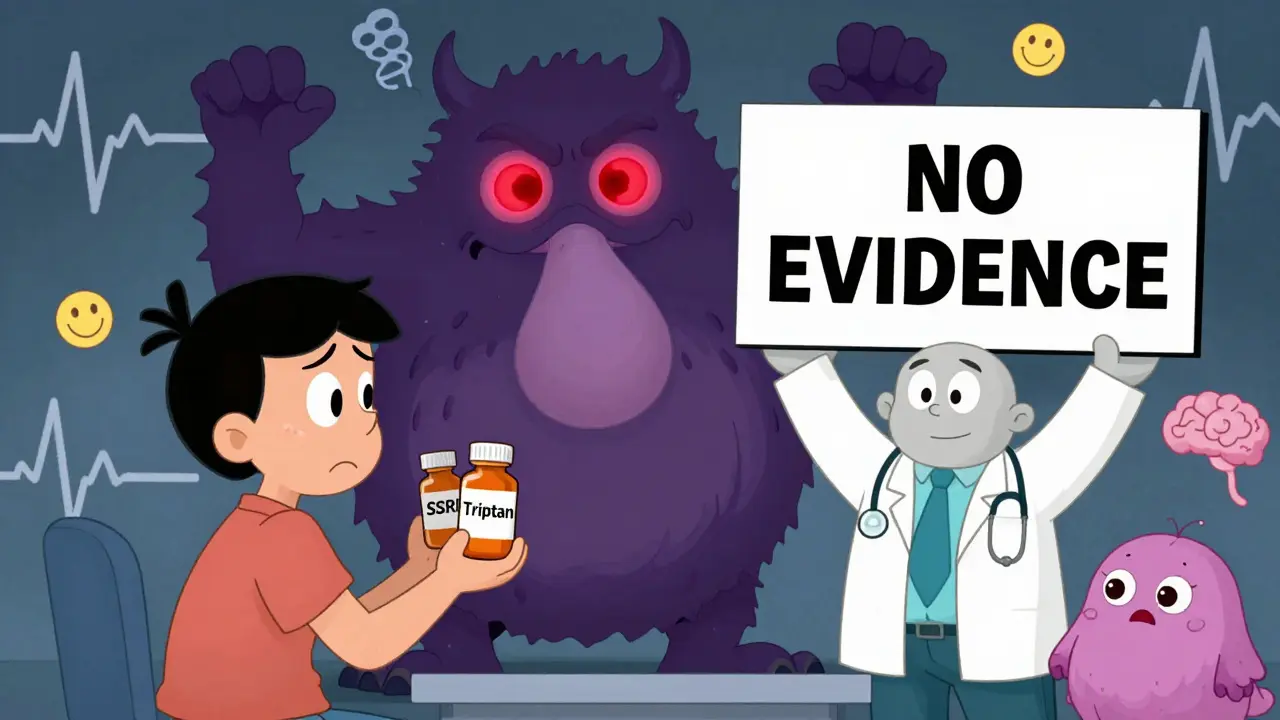
This tool helps you understand the risk of serotonin syndrome when taking certain medications together. Based on evidence from the article "Triptans and SSRIs: The Truth Behind the Serotonin Syndrome Myth".
For over 15 years, patients with migraines who also take antidepressants have been told they can’t use triptans-because it might cause serotonin syndrome. It’s a warning that shows up in pharmacy alerts, doctor’s notes, and even Reddit threads. But here’s the thing: there’s no real evidence it’s true.
What’s the big scare about?
The fear started in 2006, when the U.S. Food and Drug Administration (FDA) issued a safety alert. They worried that combining triptans (like sumatriptan or rizatriptan) with SSRIs (like sertraline or fluoxetine) could flood your brain with too much serotonin and trigger serotonin syndrome-a rare but dangerous condition that can cause shivering, confusion, rapid heart rate, and even seizures. It sounded scary. And because it involved two widely used drugs-migraine meds and antidepressants-it stuck. Millions of people were told they had to choose: treat your migraines or keep taking your antidepressant. But the warning wasn’t based on real cases. It was based on theory.How serotonin syndrome actually works
Serotonin syndrome isn’t caused by just any increase in serotonin. It’s caused by overstimulation of specific receptors-mainly 5-HT2A and, to a lesser extent, 5-HT1A. Drugs like MAOIs, certain opioids, and high-dose SSRIs can do this because they massively boost serotonin levels across the board. Triptans? They don’t work that way. They’re designed to target only two serotonin receptors: 5-HT1B and 5-HT1D. These are the ones in blood vessels and nerves that help shut down migraine pain. They barely touch 5-HT2A or 5-HT1A. Think of it like using a key that only fits one lock. Even if you’ve got a lot of keys floating around (thanks to your SSRI), the triptan key still won’t open the wrong door.The data doesn’t back the warning
In 2019, researchers from the University of Washington looked at over 61,000 patients who took triptans while on SSRIs or SNRIs. None developed serotonin syndrome. Not one. That’s not a fluke-it’s a huge sample size, covering nearly 30 years of real-world use. Even more telling? The FDA’s own adverse event database from 2006 to 2022 recorded only 18 possible cases involving triptans and SSRIs. Every single one was reviewed by experts. None were confirmed as true serotonin syndrome. Most were misdiagnosed migraines, panic attacks, or side effects from other drugs. Meanwhile, SSRIs alone carry a known risk-about 0.5 to 0.9 cases per 1,000 patient-months, mostly with certain drugs like nefazodone. But when you add a triptan? No spike. No pattern. No signal.Why the myth still survives
You’d think after 17 years of solid evidence, the warning would be gone. But it’s not. Pharmacy software still pops up alerts. Some doctors still hesitate. Patients still get turned away at the counter. A 2022 survey by the American Migraine Foundation found 42% of people taking SSRIs were denied triptans because of the supposed risk. Not because they had symptoms. Not because their doctor thought it was unsafe. Just because of a warning that doesn’t hold up. In New Zealand, the Migraine Foundation says it’s “quite common” to hear someone was told they couldn’t take a triptan because they were on an antidepressant. A 2024 article in New Zealand Doctor even ran a quiz asking if serotonin toxicity is likely with this combo. The correct answer? False.
What doctors actually do
The real story is in the clinics. A 2021 survey of 250 headache specialists found 89% routinely prescribe triptans with SSRIs or SNRIs-with no extra monitoring, no warnings, no special rules. Why? Because they’ve seen it. They’ve treated hundreds of patients. And they’ve never seen serotonin syndrome from this combo. The American Headache Society, the National Headache Foundation, and the American Academy of Neurology all agree now: don’t avoid triptans just because someone’s on an SSRI. Their 2022 consensus statement says it plainly: “Clinicians should not avoid prescribing triptans to patients taking SSRIs or SNRIs due to theoretical concerns.” Even UpToDate, the go-to clinical reference for doctors, updated its entry in July 2023 to say the risk is “negligible.”What’s changing-and what’s not
Prescribing patterns are shifting. In 2007, only 18.7% of triptan prescriptions were written alongside SSRIs. By 2022, that number jumped to 32.4%. More people are getting the treatment they need because more doctors trust the data. Pharmaceutical companies are updating labels, too. The current prescribing info for Imitrex (sumatriptan) still mentions the FDA warning-but now it adds: “Epidemiological studies have not shown an increased risk of serotonin syndrome with concomitant use.” The European Medicines Agency never issued the warning in the first place. And now, the American Headache Society has formally petitioned the FDA to remove it. A major study tracking 10,000 patients on both drugs is underway, with no cases of serotonin syndrome found so far.What this means for you
If you’re on an SSRI or SNRI and get migraines, you’re not at risk from triptans. You’re not going to accidentally poison yourself. You’re not going to end up in the ER because you took a sumatriptan tablet. You’re just someone who needs both medications-and you deserve to have them both. If a pharmacist or doctor tells you not to take them together, ask them: “What’s the evidence?” Point them to the 2019 JAMA Neurology study. Mention the American Headache Society’s guidelines. Show them the data. This isn’t about being bold-it’s about using science, not fear, to make decisions.

Comments (12)
June Richards
1 Feb, 2026OMG THANK YOU FOR THIS POST!!! I’ve been told for YEARS I can’t take sumatriptan because of my Zoloft and it made me cry every time I got denied. 😭 Now I’m gonna print this out and throw it at my pharmacist. 🙌
Jaden Green
1 Feb, 2026The FDA’s warning was never grounded in empirical rigor-it was a knee-jerk reaction born of pharmacological anxiety and liability aversion. The 2019 JAMA Neurology study, with its 61,000-patient cohort, represents a paradigmatic refutation of the myth, yet institutional inertia persists because cognitive dissonance is cheaper than protocol revision. The fact that UpToDate updated its entry in 2023 is a minor victory, but the real tragedy lies in the $450M annual waste on inferior therapeutics-this isn’t just misinformation, it’s medical malpractice by omission.
Nidhi Rajpara
2 Feb, 2026I am from India and I have been taking sumatriptan with escitalopram for 8 years. No issue at all. The warning is outdated and not based on evidence. Many doctors here still follow it blindly. It is unfortunate. Please share this with more people.
Rachel Liew
4 Feb, 2026I’m so glad someone finally said this. I’ve had migraines since I was 16 and anxiety since I was 21. I was terrified to take triptans because my old doctor scared me. Now I’m on both and I feel like a human again. Thank you for the science, not the fear.
Melissa Melville
5 Feb, 2026So let me get this straight… we’ve got a $450 million dollar mistake because someone at the FDA got spooked by a theory? And now we’re all supposed to be grateful when a doctor finally remembers how to Google? 🤦♀️
Deep Rank
6 Feb, 2026Honestly? This whole thing is just another example of how medicine loves to scare people more than it loves to help them. I had a panic attack once after taking a triptan and my doctor blamed the combo. Turns out I was just stressed and dehydrated. But now I’m labeled ‘high risk’ and my insurance won’t cover my meds unless I jump through 17 hoops. It’s not science. It’s bureaucracy with a stethoscope.
Naomi Walsh
7 Feb, 2026I’m shocked this is even a debate. The European Medicines Agency never bought into this nonsense. The American Headache Society published a consensus in 2022. The data is overwhelming. Yet here we are, in 2025, still explaining basic pharmacology to people who should know better. It’s not ignorance-it’s institutional cowardice.
Bryan Coleman
9 Feb, 2026I’m a nurse in a headache clinic. We’ve prescribed this combo to over 800 patients. Zero cases of serotonin syndrome. The only thing we’ve seen? People finally sleeping again, going to work, and not crying in the parking lot before their appointments. This isn’t risky. It’s restorative.
Naresh L
9 Feb, 2026It’s interesting how fear becomes doctrine when it’s wrapped in authority. The FDA didn’t say ‘this causes serotonin syndrome’-they said ‘it might.’ And ‘might’ became ‘will’ in the minds of pharmacists and doctors. We’ve built a culture where theoretical risk outweighs lived experience. Perhaps the real syndrome here is the inability to unlearn something that was never true.
Sami Sahil
10 Feb, 2026Bro this is life changing. I was about to give up on triptans. Now I’m gonna call my doc tomorrow and say ‘show me the evidence.’ If they can’t, I’m getting a second opinion. You’re a legend for posting this.
franklin hillary
11 Feb, 2026This is the most important post I’ve read all year. Migraine sufferers are already fighting a war against pain. Depression is a second front. And now we’re being told we can’t use the weapons we need because of a ghost story from 2006? This isn’t caution. This is cruelty dressed up as care. The FDA needs to apologize. Not just update a label. APOLOGIZE.
Bob Cohen
12 Feb, 2026I work in pharmacy. I used to pop that alert every time. Now I just say ‘Here’s the evidence. Let me know if you want me to call the doctor.’ Turns out most docs are thrilled to have the backup. The real villain? The software that doesn’t let us turn off the warning. We’re stuck playing by rules that don’t exist anymore.