September 2023 Pharmacy Guide – What You Need to Know
Welcome to our September roundup. We’ve collected five fresh posts that cut straight to the chase on drugs you might be taking or have heard about. Each piece is short, practical, and focused on what matters for your daily health decisions.
Spotlight on Mental Health and Pulmonary Hypertension
First up, ambrisentan. This medicine treats pulmonary arterial hypertension (PAH), but many users wonder if it affects mood. Our article breaks down real‑world experiences and points out signs of depression you shouldn’t ignore—persistent sadness, loss of interest, or sudden fatigue. It also shares simple steps you can take right now: keep a daily mood journal, set up a weekly check‑in with your cardiologist, and consider a therapist who understands chronic illness. Catching mood changes early can keep your treatment effective and your life balanced.
Nutrition Meets Medication
Valproic acid is a go‑to drug for seizures and mood disorders, yet what you eat can change how it works. We explain which nutrients boost its effectiveness and which may cause side effects. For example, steady protein intake helps maintain stable blood levels, while very high‑fat meals can increase liver strain. We also flag common culprits—like grapefruit juice—that can interfere with drug metabolism. At the end of the post you’ll find a quick grocery list that pairs valproic‑friendly foods (lean meats, whole grains, leafy greens) with easy meal ideas.
Next, we look at midodrine, the blood‑pressure pill often prescribed for orthostatic hypotension. Long‑term use raises questions about safety, especially the risk of excessive vasoconstriction that could raise blood pressure too high when you stand or sit. Our guide highlights common concerns—headaches, scalp tingling, or a sudden rise in resting blood pressure—and offers practical monitoring tips. Simple home checks, like measuring standing and sitting blood pressure once a week, can catch problems early. If you notice a pattern, jot it down and bring it to your doctor’s next appointment.
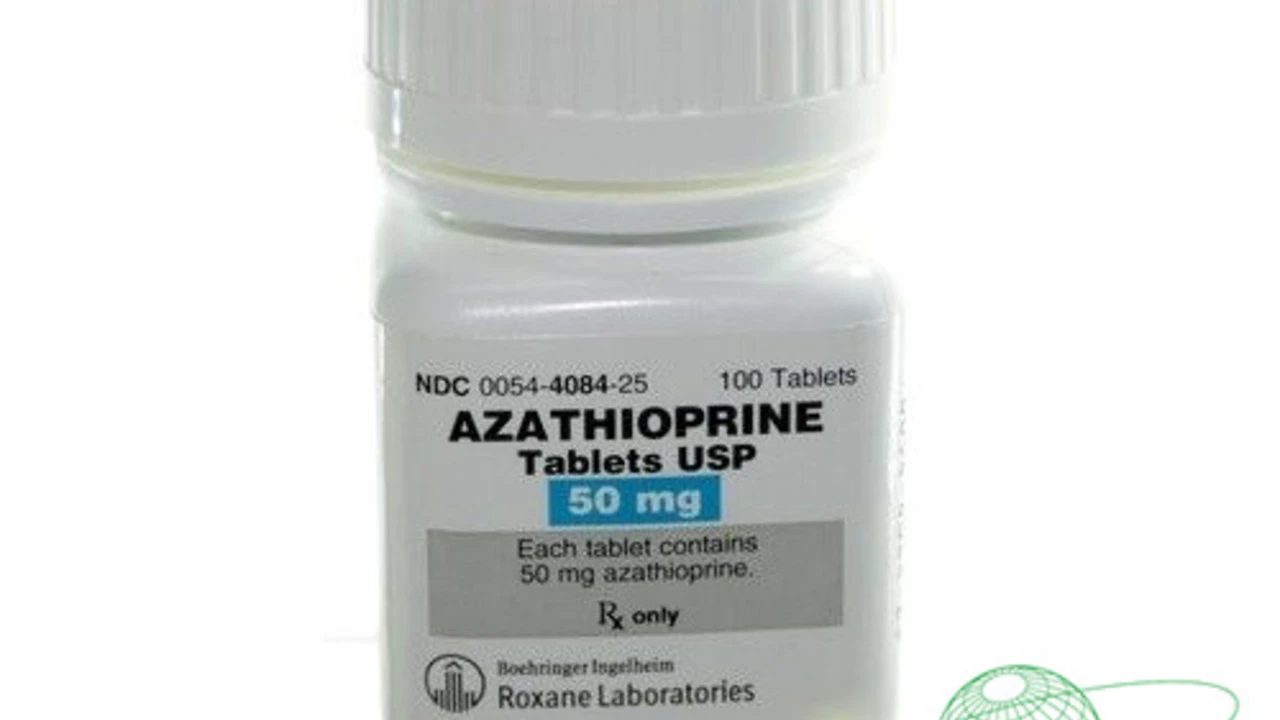
Azathioprine allergies are another hot topic. This immunosuppressant can trigger skin rashes, fever, or even liver issues in sensitive people. We walk you through the warning signs: red patches that don’t fade, unexplained bruising, or unusual fatigue after the first few weeks of therapy. The key takeaway? If you notice any new reaction, stop the drug only after consulting a healthcare professional and consider allergy testing. Early detection can prevent serious complications and give your doctor time to adjust the dose or switch medications.
Finally, we explore simethicone for pancreatitis relief. While simethicone is known for easing gas, its role in soothing pancreatic inflammation isn’t widely discussed. Our article sums up the limited evidence—some patients report reduced abdominal bloating and mild pain after taking an over‑the‑counter dose, but it never replaces enzyme replacement or prescribed anti‑inflammatory drugs. We stress that you should always run any new supplement by your gastroenterologist, especially if you’re dealing with acute or chronic pancreatitis.
Each post aims to give you actionable info without the jargon. Whether you’re managing a chronic condition, tweaking your diet, or simply staying informed, these September entries are designed to fit into a busy life. Bookmark the topics that matter most, and feel free to revisit them whenever you need a quick refresher. Your health decisions become easier when you have clear, concise facts at your fingertips.