GLP-1 Side Effect Tracker
Track Your Symptoms
Your Progress Timeline
Personalized Guidance
Your Status
Recommended Actions
When you hear about GLP-1 receptor agonists like Ozempic or Wegovy, the headlines often focus on dramatic weight loss - 15%, 20%, even more. But behind those numbers is a much quieter, less talked-about reality: for a lot of people, the first few weeks feel like a battle with their own stomach. Nausea. Vomiting. Bloating. Diarrhea. Constipation. These aren’t rare side effects. They’re the norm.
More than 40% of people who start a GLP-1 agonist experience nausea. Some studies show it’s as high as 70%. And it’s not just about feeling queasy - it’s about whether you can stick with the drug long enough to get the benefits. For many, the side effects are so intense they quit. But here’s the thing: most of these symptoms don’t last. And if you know how to manage them, you can get through them.
Why Do GLP-1 Agonists Cause Nausea and GI Problems?
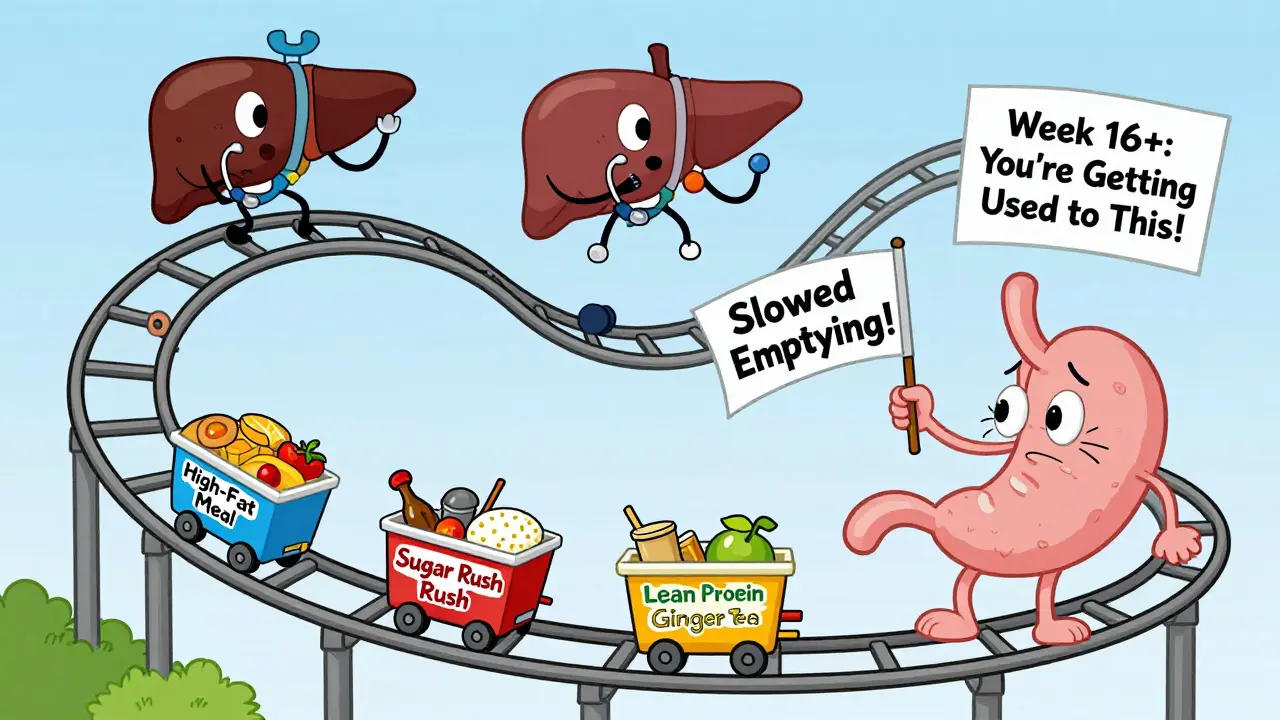
These drugs don’t just lower blood sugar - they change how your gut works. GLP-1 receptor agonists mimic a natural hormone that tells your body you’re full. That’s why you eat less and lose weight. But that same hormone also slows down how fast your stomach empties. That’s helpful for controlling hunger, but it’s a problem for digestion.
When food sits in your stomach longer than usual, it can cause bloating, discomfort, and nausea. Your gut muscles don’t move food along the way they used to. That’s why constipation happens. Or sometimes, your intestines overreact, and you get diarrhea. It’s not a bug - it’s the drug doing exactly what it’s supposed to do. The side effects are a direct result of the mechanism.
It doesn’t matter if you’re on semaglutide, liraglutide, or tirzepatide. All of them slow gastric emptying. That’s why nausea is a class-wide effect. Whether it’s a weekly injection or a daily pill, the gut feels it.
When Do Side Effects Start - And When Do They Go Away?
The worst of it usually hits during the dose-escalation phase. That’s when your doctor slowly increases your dose over weeks to help your body adjust. For most people, nausea peaks in the first 2 to 4 weeks. It’s not fun. But if you stick with it, things get better.
Studies show that by the time you reach your maintenance dose - usually around week 16 to 20 - nausea drops significantly. In clinical trials, about 15-20% of people on semaglutide still had nausea at full dose. For liraglutide, it was closer to 20-25%. That’s still noticeable, but far better than the 40-70% during ramp-up.
Real-world experience backs this up. On Reddit threads like r/Ozempic and r/Wegovy, users say the same thing: "Week 1 was hell. Week 4, I felt okay. Week 8, I forgot I was even on it." The key? Time. Your gut adapts. But you have to give it that time.
What Are the Real Risks - Beyond Nausea?
Most GI side effects are mild. But not all. There are serious, though rare, complications you need to watch for.
A 2023 study in JAMA Network looked at over 5,000 people on GLP-1 drugs and compared them to those on other weight-loss meds. The results were clear: GLP-1 agonists increased the risk of:
- Pancreatitis - 9 times higher risk
- Bowel obstruction - 4 times higher risk
- Gastroparesis (stomach paralysis) - 3.7 times higher risk
These aren’t everyday occurrences. But they’re real. And they’re not random. They happen because the gut is being slowed down - sometimes too much. If you can’t pass gas, haven’t had a bowel movement in days, or have severe, constant abdominal pain, that’s not normal nausea. That’s a red flag.
Other serious signs to watch for:
- Yellowing skin or eyes (jaundice)
- Severe vomiting and diarrhea that won’t stop
- Sharp pain in your upper abdomen
- Dark urine or extreme fatigue
If you have any of these, call your doctor. Don’t wait. There’s also a boxed warning from the FDA about thyroid tumors in animals - no confirmed cases in humans, but it’s why these drugs aren’t approved for people with a personal or family history of thyroid cancer.
How to Reduce Nausea and GI Side Effects
You don’t have to suffer through this. There are proven ways to make it easier.
1. Go slow with dosing. Your doctor should be increasing your dose gradually. If they’re not, ask. Rushing the escalation makes side effects worse. Give your body 2-4 weeks between dose increases. Don’t skip steps.
2. Eat smaller meals. Large meals = more nausea. Try 4-5 small meals instead of 3 big ones. Even if you’re not hungry, eat something light. Skipping meals can make nausea worse.
3. Avoid high-fat and sugary foods. These are the worst offenders. Fried food, creamy sauces, pastries, soda - they sit in your stomach and make everything feel heavier. Stick to lean proteins, vegetables, whole grains, and broth-based soups.
4. Stay hydrated - but sip slowly. Chugging water right after eating can trigger nausea. Sip water throughout the day. Try ginger tea or peppermint tea. Ginger is a natural anti-nausea remedy.
5. Don’t lie down after eating. Gravity helps digestion. Stay upright for at least 30 minutes after a meal. Don’t nap or binge-watch TV right after dinner.
6. Consider timing. Some people find taking the dose at night helps. Your stomach is less active while you sleep, and you’re not eating afterward. Try it - if nausea hits during the day, switching to bedtime might help.
7. Talk to your doctor about OTC options. Medications like dimenhydrinate (Dramamine) or meclizine can help with nausea. But don’t self-prescribe. Ask your doctor first. Some anti-nausea drugs interact with GLP-1 agonists.

What If You Can’t Tolerate It?
It’s okay to stop. If the side effects are unbearable, or if you’re losing weight too fast and feeling dizzy or weak, talk to your doctor. You don’t have to push through pain.
Some people switch to a different GLP-1 agonist. Others try a lower dose longer. A few go off entirely. There’s no shame in that. These drugs aren’t magic pills. They’re tools. And if they’re making you feel worse than you did before, they’re not helping.
Also, remember: weight loss isn’t the only benefit. For people with type 2 diabetes, these drugs lower blood sugar, reduce heart disease risk, and protect kidney function. If you’re using it for diabetes, the benefits might still outweigh the side effects - if you can manage them.
The Bigger Picture: Why These Drugs Are Still Growing
Despite the side effects, the market for GLP-1 agonists is exploding. It was worth $15 billion in 2022. By 2028, it could hit $44 billion. Why? Because they work. In clinical trials, semaglutide led to an average weight loss of 14.9% over 68 weeks. Placebo? Just 2.4%.
People aren’t just using them for weight loss anymore. They’re used for diabetes, prediabetes, fatty liver disease, and even heart failure. The science behind them is solid. The side effects are real. But they’re manageable.
Doctors are learning how to prescribe them better. Newer versions are being tested with slower-release systems and combination formulas to reduce GI upset. In the next few years, we’ll likely see options that give the same benefits with less nausea.
For now, the message is simple: don’t panic. Don’t quit too soon. But don’t ignore warning signs. Use the strategies above. Talk to your provider. And give your body time to adjust. Most people who stick with it for 3 months say the side effects become a distant memory - and the results, worth it.
How long does nausea last on GLP-1 agonists?
Nausea typically peaks during the first 2 to 6 weeks, especially while your dose is being increased. Most people notice significant improvement once they reach their maintenance dose, which usually happens after 16 to 20 weeks. For about 60-70% of users, nausea becomes mild or disappears entirely by week 12. Persistence is key - the side effects are usually temporary.
Can I take anti-nausea medicine with Ozempic or Wegovy?
Yes, but only under medical supervision. Over-the-counter options like dimenhydrinate (Dramamine) or meclizine are sometimes used to help with nausea. Ginger supplements or tea may also help. However, some anti-nausea drugs can interact with other medications or affect how your body absorbs the GLP-1 agonist. Always check with your doctor before adding anything new.
Do all GLP-1 agonists cause the same side effects?
Yes, gastrointestinal side effects are common across the entire class. Whether it’s semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), or tirzepatide (Mounjaro), they all slow gastric emptying. That’s why nausea, bloating, constipation, and diarrhea are class-wide effects. The severity may vary slightly - for example, semaglutide tends to cause less nausea at maintenance dose than liraglutide - but the mechanism is the same for all.
Should I stop taking my GLP-1 agonist before surgery?
Yes. Because GLP-1 agonists slow digestion, they increase the risk of aspiration during anesthesia. Most surgeons and anesthesiologists recommend stopping the medication at least 1 week before any procedure requiring sedation. Always inform your surgical team that you’re on a GLP-1 agonist - this is a critical safety step.
Are GI side effects worse with higher doses?
Yes. Higher doses - like those used for weight loss (Wegovy) - tend to cause more gastrointestinal side effects than lower doses used for diabetes (Ozempic). This is why doctors start with the lowest possible dose and increase slowly. If you’re on a higher dose and struggling, talk to your provider. You may benefit from staying at a lower dose longer, or switching to a different medication.


Comments (15)
Jack Havard
12 Feb, 2026I've been on Ozempic for 10 weeks. Nausea? Barely noticeable. But my bowel movements have turned into a science experiment. I'm not saying it's bad, just that nobody talks about the constipation that lasts longer than your last relationship.
Sonja Stoces
14 Feb, 2026I'm not saying Big Pharma is behind this... but why do all these drugs have the same side effects? Coincidence? Or is it because they all came from the same lab? 🤔
Luke Trouten
16 Feb, 2026It's fascinating how the body adapts. The gut isn't broken-it's recalibrating. What we call 'side effects' might just be the system adjusting to a new regulatory paradigm. Patience isn't passive; it's physiological.
Kristin Jarecki
17 Feb, 2026As a clinical pharmacist, I must emphasize: the risk-benefit profile of GLP-1 agonists remains strongly favorable for appropriate candidates. While GI adverse events are common, they are typically transient and manageable with proper patient education and titration protocols.
Jonathan Noe
19 Feb, 2026Look, I've seen people quit after week 2 because they didn't like feeling full. Bro, that's the whole point. You're not supposed to eat like you're at an all-you-can-eat buffet anymore. If you're still craving fries after 3 weeks, maybe the drug is working better than you think.
Jim Johnson
21 Feb, 2026I started at the lowest dose and went super slow-6 weeks between each increase. Nausea? Gone by week 5. I eat like a bird now, but I'm not miserable. Seriously, if you're in pain, talk to your doc. But if you're just uncomfortable? You're probably doing it right.
Vamsi Krishna
21 Feb, 2026In my village in Kerala, we used to treat nausea with ginger, turmeric, and a good scolding from grandma. Now we inject synthetic hormones and call it medicine. Progress? Or just expensive placebo with side effects? I've seen both. The body remembers what the lab forgot.
Brad Ralph
23 Feb, 2026Nausea is just your gut saying "I didn't sign up for this." 🤷♂️
christian jon
23 Feb, 2026I've had three family members on these drugs. One had pancreatitis. One lost 50 pounds and now looks like a ghost. One quit after 2 weeks and said, "I'd rather be fat and healthy than skinny and terrified." And you know what? She's right. This isn't health-it's a cosmetic experiment with a 9x higher risk of pancreatitis. Who approved this?
Suzette Smith
25 Feb, 2026I was skeptical too, but after 4 months, I'm not nauseous anymore. I just feel... lighter. Not just physically. Like I can breathe better. Weird, right?
Autumn Frankart
25 Feb, 2026This is all part of the plan. The FDA knows. The doctors know. The pharma reps know. They want you to suffer so you’ll keep taking it. Why? Because the longer you stay on it, the more they make. And if you quit? They just sell it to someone else. Wake up.
Pat Mun
26 Feb, 2026I started this journey thinking it was just about weight loss. But honestly? It changed how I think about food. I used to eat out of boredom, stress, habit. Now, I pause. I ask: "Do I need this?" And sometimes, the answer is no. That’s not a side effect-that’s a life upgrade. I still get bloated sometimes, but I’d rather be bloated and aware than stuffed and numb.
Skilken Awe
28 Feb, 2026The gastric emptying delay isn't a side effect-it's a pharmacodynamic endpoint. If you're experiencing GI distress, you're not non-compliant; you're pharmacologically responsive. The issue isn't the drug. It's the lack of predictive biomarkers for individualized titration. We're still in the Stone Age of personalized dosing.
andres az
28 Feb, 2026They say it's temporary. But what if it's not? What if your gut never recovers? What if you're stuck with slow digestion for life? No one mentions that. They just show before-and-after pics. Where's the after-after? The guy who's 60 pounds lighter but can't eat a burger without a 3-hour recovery period?
Steve DESTIVELLE
1 Mar, 2026The body is a river. The drug is a dam. The nausea is the water trying to find its way. You cannot force the river. You cannot rush the dam. You must wait. The water will flow. The river will change. But the river remembers. And so will you.